Introduction
Cupping therapy, a traditional technique involving the application of cups to create localised negative pressure on the skin, has been utilised for over four thousand years [1]. Its use spans various conditions, including herpes zoster, hypertension, stroke, cough, asthma, and, notably, musculoskeletal pain [1, 2]. The athletic community has recently shown a burgeoning interest in this modality for its potential in muscle recovery and pain management [3].
Athletes across multiple disciplines strive for optimal performance and swift recovery, often turning to various rehabilitation modalities post-exercise, training, and competition [4-6]. Cupping therapy can be pivotal, potentially outperforming other techniques such as massage and cryotherapy. It is acclaimed for enhancing local blood flow, fostering microcirculation, facilitating endothelial cell repair, and promoting tissue regeneration processes like granulation and angiogenesis [7]. Moreover, it is believed to influence skin blood flow, alter biomechanical properties, elevate pain thresholds, improve local metabolism, reduce inflammation, and modulate immune cellular mechanisms [7, 8]. Cupping can alleviate muscle stiffness when applied to specific acupoints by inducing hyper-aemia or haemostasis [8].
The prevalence of musculoskeletal disorders has escalated, now a leading cause of disability globally, affecting 13.5% to 47% of the general population [7]. Athletes, in particular, are susceptible to such conditions as pain due to different injuries causing tendinopathies, sprains, strains, etc., irrespective of their sport [8]. Despite cupping therapy’s rising popularity, the scientific community is diligently working to substantiate its claimed benefits. A myriad of systematic reviews present findings, some asserting positive effects on musculoskeletal pain [9, 10]. This underscores the necessity to critically appraise the robustness of these conclusions and reconcile any conflicting recommendations.
In the athletic sphere, cupping therapy is strategically employed as part of a recovery protocol [4]. It is reportedly used with state-of-the-art training techniques, with some athletes advocating for its efficacy in reducing soreness and enhancing muscle recovery [10]. The therapy’s application ranges from post-training sessions to post-competition recovery, claiming improved functionality and healing in fatigued muscles [9]. It is also suggested for treating sports injuries and conditions like plantar fasciitis, sciatica, and frozen shoulder [2].
The literature on cupping therapy’s effects on muscle pain reveals a complex picture. Studies have explored its impact through various lenses, assessing outcomes such as pain intensity, muscle stiffness, and range of motion [11, 12]. Some research suggests that cupping may offer a non-pharmacological option for pain management, with evidence pointing to its effectiveness in managing chronic pain, knee osteoarthritis (KOA), low back pain, neck pain, and conditions like herpes zoster [1, 11, 12]. However, the quality of evidence ranges from very low to moderate, indicating a need for more rigorous studies to establish its efficacy conclusively [2, 3]. This study aims to synthesise the evidence from systematic reviews examining the effectiveness of cupping therapy for musculoskeletal pain in the general population and athletes. It will also identify trends and gaps in specific physical therapy modalities, such as cupping therapy, within the existing literature to help stakeholders prioritise future research.
Materials and methods
Literature search
This systematic review was registered on Prospero under registration number CRD42022359262. We adhered to the PRISMA checklist to report this umbrella review. Our four-stage process assessed the appropriateness of systematic review conclusions by comparing research questions, types of primary studies, levels of evidence, and methodological quality.
Eligibility criteria
Eligible studies were systematic reviews of randomised controlled trials published in English involving human participants who received cupping therapy for musculoskeletal pain, pain pressure thresholds, or disability. We excluded reviews combining cupping therapy with other interventions and non-English publications, as these often report over-optimistic results [13, 14].
Search strategy
We refined our search strategy to include both the general and athletic populations. Using the Population, Intervention, Comparator, and Outcome (PICO) model, we crafted the guiding question: “What is the effectiveness of cupping therapy compared to other interventions (e.g., heat therapy, usual care, conventional medications, or no treatment) in reducing musculoskeletal pain across different populations?” Searches were conducted in PubMed, Web of Science, Scopus, MEDLINE, Cochrane Central, CINAHL, EMBASE, and PEDro until May 2023.
The search strategy for this umbrella review was initially executed through May 2023. We acknowledge that the time elapsed since the initial search may have led to the publication of additional systematic reviews that could influence our findings. So, we updated the search strategy and search process on 18 August 2024 to include any additional published studies. The old and new search strategies are presented in the Supplementary file.
Study selection
Two independent researchers (GI and MM) screened the titles and abstracts of the retrieved articles for eligibility. The full texts of the preliminarily selected articles were then reviewed to confirm that they met the inclusion criteria. Elected articles were further analysed to extract the required information, including the first author’s name, year of publication, target population, number of included studies, number of participants, methodological quality, results, and author’s conclusions. If there was no consensus around study selection, a constructive debate ensued with a third author (ME) until a consensus was reached.
Methodological quality
The methodological quality of the systematic reviews was assessed using the AMSTAR2 checklist [1]. Two reviewers (PN and ME) evaluated the studies based on 16 yes/no questions, with critical domains identified. The items two (Protocol registered before the commencement of the review), four (Adequacy of the literature search), seven (Justification for excluding individual studies), nine (Risk of bias from individual studies being included in the review), eleven (Appropriateness of meta-analytical methods), thirteen (Consideration of risk of bias when interpreting the results of the review), and seventeen (Assessment of pres ence and likely impact of publication bias) are considered critical domains. The overall confidence in the results was classified as high, moderate, low, or critically low based on identified weaknesses and flaws.
Evaluating the certainty of the evidence In addition to evaluating the methodological quality of the included systematic reviews using the AMSTAR 2 tool, we also conducted a GRADE assessment for each of the included studies. The GRADE approach was used to assess the certainty of the evidence, considering factors such as risk of biases, inconsistencies, indirectness, imprecision, and publication bias [15]. This enabled us to provide a more comprehensive evaluation of the quality of evidence and reliability of the conclusions drawn from the synthesised data.
Results
Identification and selection of studies
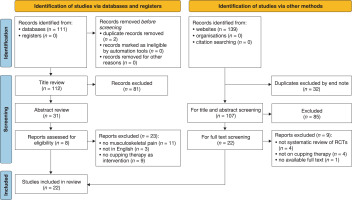
Table 1 explains the summary characteristics of the included studies. A total of 21 systematic reviews, including 301 studies that fulfilled the eligibility criteria and included 27,960 participants, were evaluated [16-36]. Seventeen of these reviews were published after 2016. Figure 1 presents the flow diagram for the inclusion and exclusion of the studies.
Table 1
Summary of the characteristics of the studies
| Author, year | Population | Number of studies and participants | Methodological quality of the included studies | Main results | Author’s conclusions |
|---|---|---|---|---|---|
| Bridgett et al. 2017 [16] | Athletes from different sports and levels of practice | 5 studies (190 participants) | Low quality | Cupping is better than no intervention for reducing lower back and hip pain in soccer players. It is also effective in reducing injury-induced disability caused by lower back pain in soccer players. Cupping is more effective than no intervention in terms of lumbar isometric endurance. Additionally, perceived exertion after training is lower with cupping compared to no intervention controls. Creatine kinase values are also reduced 16 hours after cupping compared to no intervention, making cupping a valuable addition to training regimens. | Insufficient data and methodo logic flaws prevent a definitive recommendation for or against cupping in athletes. More studies are needed to determine its effectiveness, safety, and mechanisms. |
| Cao et al. 2014 [17] | Participants with chronic neck pain, non-specific low back pain, osteoarthritis, carpal tunnel syndrome, acute ankle sprain, and headache | 10 (578 participants) | Moderate quality | A meta-analysis of two trials showed that four weeks of dry cupping We found that cupping is more therapy reduced pain (VAS) by -1.85 cm (95% CI: -2.66 to -1.04,effective in reducing short-term p < 0.001, 2 trials, 86 participants) and improved QoL (SF-36 mental pain than other treatments. MD = 5.90, 95% CI: 0.16 to 11.64, p = 0.04, I2 Z 50%; SF-36 physical However, we could not determine = 3.77, 95% CI: 1.27 to 6.26, p = 0.003, 2 trials, 86 participants). mine its specific effects on chronic Wet cupping therapy was also effective in reducing pain (VAS MD = or acute pain due to limited trials. -7.07 cm, 95% CI: -7.45 to -6.69, p < 0.001, 61 participants) and was even more effective than conventional drugs for pain reduction. Wet cupping therapy was found to be more effective in reducing pain than heat therapy after 1-2 weeks of treatment. Two trials showed that wet cupping and moving and dry cupping therapy were more effective than usual care in reducing pain after 2 weeks of treatment. However, two trials reported no significant differences between moving cupping and progressive muscle relaxation after 12 weeks of treatment. Out of the six trials, one showed a significant difference between moving cupping therapy and usual care in improving QoL physical scores after two weeks of treatment. | |
| Moura et al. 2018 [18] | Participants with chronic back pain | 16 studies (1049 participants) | Low quality | Cupping therapy was more effective than the control group in reducing pain, with a difference between means of -1.59 [95% CI: -2.07 to -1.10]; p = 0.001. Moderate to high heterogeneity was observed (I2 = 67.7%, p = 0.001). | Cupping therapy shows promise in treating chronic back pain in adults by reducing pain intensity scores. However, limited findings are due to the high heterogeneity and median methodological quality of RCTs. |
| Cramer et al. 2020 [19] | Participants with neck pain, knee osteoarthritis, low back pain, brachialgia, carpal tunnel syndrome, or fibromyalgia, myofascial pain syndrome | 18 studies (1172 participants) | Moderate quality | Cupping therapy was found to significantly reduce short-term pain intensity when compared to no treatment (SMD = 1.03; 95% CI: 1.41 to 0.65), but not compared to sham cupping (SMD = 0.27; 95% CI: 0.58 to 0.05), or other active treatments (SMD = 0.24; 95% CI: 0.57 to 0.09). For disability, cupping had medium-sized short-term effects compared to no treatment (SMD = 0.66; 95% CI: 0.99 to 0.34) and other active treatments (SMD = 0.52; 95% CI: 1.03 to 0.0028), but not compared to sham cupping (SMD = 0.26; 95% CI: 0.57 to 0.05). Cupping was superior to no treatment for neck pain but not for lower back pain. Dry cupping and pulsating/pulsatile cupping were more effective in reducing disability than no treatment, but wet cupping did not show significant results. | Cupping may be a viable treatment for chronic pain; however, limited evidence exists due to clinical heterogeneity and potential bias. |
| Kim et al. 2011 [20] | LBP and acute trigeminal neuralgia | 2 studies (115 participants) | Low quality | Two RCTs comparing cupping therapy to other pain relief methods showed significant pain reduction. One RCT found dry cupping more effective than non-steroidal anti-inflammatory drugs for non-specific low back pain. Another RCT found wet cupping more effective than analgesics for acute trigeminal neuralgia. | Our review suggests cupping may help manage pain, but the low number of analysed RCTs and their quality make firm conclusions impossible. |
| Seo et al. 2021 [21] | Migraine | 3 studies (210 participants) | Low quality | Wet cupping is more effective than drugs in treating migraines, according to several studies. Jiang’s (60 participants) and Song’s (90 participants) studies showed significant improvement in wet cupping compared to drugs using VAS and migraine scores. Similarly, Chen’s study (60 participants) found wet cupping to be more effective than drugs using VAS MF, MI, HD, and MAS. | Cupping therapy may have therapeutic effects on migraines. Larger and more rigorously designed RCTs are needed to confirm. |
| Wood et al. 2020 [22] | LBP, upper shoulder and neck pain, hamstrings and ITB flexibility, fibromyalgia, Knee OA, chronic neck pain, and non-specific neck pain | 18 studies (930 participants) | Moderate quality | Dry cupping, an alternative therapy, significantly reduces chronic neck (MD = -21.67; 95% CI: -36.55, to -6.80) and low back pain (MD = -19.38; 95% CI: -28.09, to -10.66). It also improves functional status (MD = -4.65; 95% CI: -6.44 to -2.85) and range of motion (SMD = -0.75; 95% CI: -0.75 to -0.32), but the evidence is moderate to low quality. | Dry cupping effectively reduces chronic neck pain and non-specific low back pain. Adverse events are mild to moderate and resolve within 48 hours. More research is required to determine the effectiveness and safety of dry cupping for musculoskeletal pain. |
| Zhang et al. 2017 [23] | Cervical spondylosis, Knee OA, LCFN, lumbar disk herniation, scapulohumeral periarthritis, muscle fibrositis, soft tissue contusion, acute lumbar sprain, fibromyalgia, and acute ankle sprain. | 20 studies (2572 participants) | Moderate quality | Cupping and acupuncture showed no significant difference in symptom improvement for specific conditions. In cervical spondylosis, cupping was more effective in pain relief; however, data could not be pooled due to the statistical heterogeneity (I2 = 93%). Cupping also had better effects in improving the symptom improvement rate compared to acupuncture (RR = 1.13, 95% CI: 1.01 to 1.26, p = 0.04, I2 = 67%; n = 646, 6 trials). The symptom improvement rate of cupping therapy was 10% higher than acupuncture (RD 0.1, 95% CI: 0.01 to 0.19, p = 0.03, I2 = 67%; n = 646, 6 trials). In lateral femoral cutaneous neuritis, there was no significant difference between the two therapies (RR 1.10, 95% CI 1.00 to 1.22, p = 0.71, n = 100, 2 trials; RD = 0.10, 95% CI: 0.10 to 0.19, p = 0.71, n = 100, 2 trials). In scapulohumeral periarthritis, cupping was 22% more effective in improving symptoms than acupuncture. | Cupping therapy and acupuncture have similar effects in relieving pain and improving symptoms of pain-related conditions. However, more extensive and well-designed studies are necessary to confirm this conclusion. Economic evaluations could be conducted to compare the cost-effectiveness of these therapies in the future. |
| Li et al. 2017 [24] | Patients with knee osteoarthritis (KOA) | 7 studies (661 participants) | Low quality | Cupping therapy combined with Western medicine significantly improved WOMAC scores for pain [MD = -1.01,95% CI: -1.61 to -0.41, p < 0.01], stiffness [MD = -0.81, 95% CI: -1.14 to -0.48, p < 0.01], and physical function [MD = -5.53, 95% CI: -8.58 to -2.47, p < 0.01]. | Only weak evidence supports the efficacy of cupping therapy for improving treatment outcomes in KOA. Further rigorous trials are needed. |
| Ma et al. 2018 [25] | Patients with ankylosing spondylitis | 5 studies (564 participants) | low methodological quality | Participants in the cupping therapy plus Western medicine group showed significantly greater improvements (RR = 1.13, 95% CI: 1.06, 1.22, p < 0.01) with low heterogeneity χ2 = 2.88, p = 0.41, I2 = 0%). Moreover, when compared with Western medicine alone, meta-analysis indicated favourable statistically significant effects of cupping therapy plus Western medicine on the Bath Ankylosing Spondylitis Functional Index (MD = -16.63, 95% CI: -17.75 to -15.51, p < 0.01) and Bath Ankylosing Disease Activity Index (MD = -9.93, 95% CI: -10.34 to -9.52, p < 0.01), with low heterogeneity (χ2 = 0.32, p = 0.85, I2 = 0 in BASFI; (χ2 = 2.46, p = 0.29, I2 = 19% in BASDAI). Furthermore, when compared with Western medicine alone, the meta-analysis demonstrated statistically significant effects of cupping therapy plus Western medicine on the serum levels of ESR (MD = -1.28, 95% CI: -1.44 to -1.13, p < 0.01) and CRP (MD = -3.97, 95%CI: -4.71 to -3.22, p < 0.01), with low heterogeneity (χ2 = 0.50, p = 0.78, I2 = 0% in the serum level of ESR; χ2 = 0.19, p = 0.91, I2 = 0% in the serum level of CRP) | Preliminary evidence supports the hypothesis that cupping therapy can effectively improve the treatment efficacy and physical function in patients with AS. |
| Mohamed et al. 2023 [26] | Patients with musculoskeletal and sports conditions (including musculoskeletal dysfunction, sports injuries, low back pain, cervical pain, neck pain, plantar fasciitis, stiffness of soft tissues, fibromyalgia, myofascial pain syndrome, osteoarthritis, muscle fatigue, or muscle soreness) | 22 studies (1143 participants) | Moderate quality | The evidence of cupping increasing soft tissue flexibility is moderate, decreasing low back pain or cervical pain is low to moderate, and treating other musculoskeletal conditions is very low to low. The incidence of adverse events is very low. | Cupping therapy has low to moderate evidence in musculoskeletal and sports rehabilitation and might be used as a useful intervention because it decreases the pain level and improves blood flow to the affected area with low adverse effects. |
| Salazar-Méndez et al. 2023 [27] | Adult patients with fibromyalgia | 2 studies (155 participants) | Low quality | Large effect sizes were found for pain intensity MD 1.12 higher (0.43 lower to 1.46 higher), moderate effect sizes for quality-of-life MD = 0.34 lower (0.75 lower to 0.07 higher), and low effect sizes for the impact on fibromyalgia MD = 0.09 higher (0.49 lower to 0.32 higher) and sleep disorders MD = 0.13 higher (0.54 lower to 0.27 higher). | There is a discrepancy in the efficacy of cupping therapy in improving pain intensity, quality of life, sleep disturbances, and disease impact in people with fibromyalgia. Future high-quality randomised clinical trials are required. |
| Wang et al. 2018 [28] | Patients with knee osteoarthritis (KOA) | 5 studies (535 participants) | High risk of bias | Dry cupping therapy plus Western medicine significantly reduced pain scores (MD = -1.79, 95% CI: -2.40 to -1.18, p < 0.01) and improved physical function; wet cupping also showed significant improvement in LAI (MD = -3.44, 95% CI: -4.21 to -2.68, p < 0.01). | While cupping therapy shows promise in treating KOA, the evidence is weak due to high risk of bias in the included studies. More rigorous trials are necessary. |
| Wang et al. 2017 [29] | Patients with low back pain | 6 studies (458 participants) | Moderate quality | The results showed that cupping therapy was superior to control management with respect to VAS scores (SMD = - 0.73, 95% CI: -1.42 to - 0.04], p = 0.04) and ODI scores (SMD = -3.64, 95% CI: - 5.85 to -1.42, p = 0.001). There were no statistically significant differences in regard to MPPI scores. No serious adverse event were reported in the included studies. | Cupping therapy can significantly decrease the VAS scores and ODI scores in patients with LBP compared to the control management. High heterogeneity and risk of bias existing in studies limit the authenticity of the findings. |
| Yuan et al. 2015 [30] | Patients with Neck Pain and Low Back Pain (LBP) | 75 studies (11077 participants) | Low to moderate quality | Acupuncture was more effective than sham acupuncture in reducingpain immediately post-treatment for CNP (visual analogue scale (VAS) 10 cm, mean difference [MD = -0.58 (-0.94, -0.22), 95% confidence interval, p = 0.01], CLBP [standardised mean difference = -0.47 (-0.77, -0.17), p = 0.003], and acute LBP [VAS 10 cm, MD = -0.99 (-1.24, -0.73), p < 0.001]. Cupping could be more effective than waitlist in VAS (100 mm) [MD = -19.10 (-27.61, -10.58), p < 0.001] for CNP or medications (e.g. NSAID) for CLBP [MD = -5.4 (-8.9, -0.19), p = 0.003]. No serious or life-threatening adverse effects were found. | Acupuncture, acupressure, and cupping could be efficacious in treating the pain and disability associated with CNP or CLBP in the immediate term. Gua sha, tai chi, qigong, and Chinese manipulation showed fair effects, but we were unable to draw any definite conclusions, and further research is still needed. The efficacy of tuina and moxibustion is unknown because no direct evidence was obtained. These TCM modalities are relatively safe. |
| Zhang et al. 2024 [31] | Patients with low back pain (LBP) | 11 studies (921 participants) | Moderate to high quality | Meta-analysis showed a significant effect on pain improvement compared to medication therapy [n = 8; d = 1.8 (95% CI: 1.22 to -2.39), p < 0.001] and usual care [n = 5; d = 1.07 (95% CI: 0.21 to 1.93), p = 0.01]. Two studies demonstrated that cupping significantly mediated sensory and emotional pain immediately, after 24 h, and 2 weeks post-intervention (d = 5.49, 95% CI (4.13 to 6.84), p < 0.001). Moderate evidence suggested that cupping improved disability at the 1-6 month follow-up (d = 0.67, 95% CI: 0.06 to 1.28, p = 0.03). There was no immediate effect observed at the 2-8 week endpoint (d = 0.40, 95% CI: -0.51 to 1.30, p = 0.39). A high degree of heterogeneity was noted in the subgroup analysis (I2 > 50%). | The study emphasised that cupping surpasses medication and usual care in reducing pain. Future research should incorporate sham cupping and objective measurements to distinguish the effectiveness of negative pressure and the actual therapeutic effect on LBP. It is important to standardise the cupping protocol and establish a consensus on the cupping intervention of LBP management. |
| Cao et al. 2010 [32] | Patient undergoing TCM | 25 RCTs with 1516 participants | Unclear | A combination of acupuncture and cupping therapy was better than conventional medications for reducing pain (MD, -1.66; 95% CI: -2.14 to -1.19; p < 0.00001; I2 1/4 0% 0%), and for improving depression scores related to FM (MD, -4.92; 95% CI: -6.49 to -3.34; p < 0.00001; I2 1/4 32%). Other individual trials demonstrated the positive effects of Chinese herbal medicine on pain reduction compared with conventional medications. | TCM therapies appear to be effective for treating FM. However, further large, rigorously designed trials are warranted because of insufficient methodological rigor in the included trials. |
| Kim et al. 2018 [33] | Patients with neck pain | 18 RCTs, 1895 participant | Low | Compared with the no-intervention group, the cupping group exhibited significant reductions in pain (MD = -2.42, 95% CI: -3.98 to -0.86) and improvement in function (MD = -4.34, 95% CI: -6.77 to -1.19). Compared with the active control, the cupping group reported a significant reduction in pain (p = 0.0009) and significantly improved quality of life (p = 0.001). The group that received control treatment with cupping therapy (add-on group) displayed significant pain reduction compared to the active control group (p = 0.001). Of the 18 studies, only 8 reported occurrence of adverse events, which were mostly mild and temporary. | Cupping was found to reduce neck pain in patients compared with no intervention or active control groups or as an add-on treatment. Depending on the type of control group, cupping was also associated with significant improvement in terms of function and quality of life. |
| Shen et al. 2022 [34] | Patients with nonspecific low back pain | 10 studies for 690 patients | Moderate quality | There was a significant reduction in the pain intensity score with present pain intensity using wet cupping therapy (p < 0.01). In addition, both cupping therapy groups displayed significant Oswestry Disability Index score reduction compared to the control group (both p < 0.01). The patients with LBP have a substantial reduction by using wet cupping but have not shown a considerable decrease by using dry cupping (p = 0.19). In addition, only wet cupping therapy groups displayed a significantly improved quality of life compared to the control group. The study had very high heterogeneity (I2 > 50%). This means there is no standardisation in the treatment protocol within the randomised clinical trials. In the meta-regression, there was statistically significan evidence that the number of treatment times and intercepts were related (p < 0.01). | Wet cupping therapy effectively reduces the pain intensity of LBP. Furthermore, both dry wet cupping therapies improved the quality of life of patients with LBP.: |
| Azizkhani et al. 2018 [35] | Patient with nonspecific neck pain | 10 RCTs were included, involving 441 participants | Moderate to low | Meta-analysis of 5 trials revealed significant differences in pain relief in favour of cupping therapy compared with the control group [VAS 100 cm, MD = -0.84 (-1.22, -0.46), I2 = 54.7%]. Furthermore, a meta-analysis of 6 studies revealed that cupping therapy was clinically superior to the control group in patients with neck pain [SMD = -0.60 (-0.86, -0.35), I2 = 16.4%]. Assessment of quality of life using the SP36 questionnaire showed that cupping therapy increased the quality of life in patients with neck pain compared with the control group [SMD = -0.56 (-0.20, -0.92), I2 = 51.4%]. | This study provides some evidence that cupping therapy may improve treatment of patients with neck pain. |
| Chaoju et al. 2022 [36] | Non-specific low back pain | 13 RCTs (1088 participants) | Moderate to low | The VAS scores indicated that blood pricking and cupping were superior to the other treatments at relieving NLBP pain (MD = -1.43; 95% CI: -2.31 to 0.54; Z = 3.15; p = 0.002). The Oswestry Disability Index score of blood pricking and cupping was superior to that of the control group in terms of improving NLBP dysfunction (MD = -6.25; 95% CI: -8.37 to -4.31); Z = 5.77; p < 0.000 01). 7 RCTs mentioned no adverse reactions, while one study reported mild syncope [7% (n = 3), all in the 17-30 year group] that was gradually relieved after rest. | Blood pricking and cupping therapy can safely and effectively reduce pain and improve functional impairment in patients with NLBP. |
Characteristics of the study and qualitative synthesis
Most systematic reviews target studies investigating patients with non-specific low back pain [17, 19, 20, 22, 29-31] and KOA [17, 19, 22-24, 28], followed by fibromyalgia [19, 22, 23, 27]. Only two systematic reviews investigated the effectiveness of cupping for musculoskeletal conditions in athletes of different sports modalities and levels of competition [16, 26]. Only one systematic review was conducted to assess the efficacy of cupping for the treatment of ankylosing spondylitis [25], while one additional study has examined its use in migraines [21].
Regarding the quality of the included studies, the overall confidence in the results of the reviews was low as the quality of seven studies was low [16, 18, 20, 21, 26, 28, 30] and of moderate quality in nine studies [17, 19, 22-25, 27, 29, 31]. Among the critical items, all reviews failed to present a list of the excluded trials, eight reviews did not consider the risk of bias when presenting or discussing their results [17,18,21,23,28-31], four reviews did not use adequate methods for the meta-analysis [17, 20, 21, 26], the impact of publication bias was not investigated in seven reviews [17, 20, 22, 26, 27, 29, 31], and the absence of a planned protocol to guide the review was noted in five reviews [18, 20, 26, 28, 30]. Most reviews included trials of low quality (i.e., high risk of bias) (Table 2).
Table 2
Methodological quality of included systematic reviews
| AMSTAR2 checklist items | Bridgett et al. 2017 [16] | Cao et al. 2014 [17] | Moura et al. 2018 [18] | Cramer et al. 2020 [19] | Kim et al. 2011 [20] | Seo et al. 2021 [21] | Wood et al. 2020 [22] | Zhang et al. 2017 [23] | Li et al. 2017[24] | Ma et al. 2018 [25] | Mohamed et al. 2023 [26] | Salazar-Méndez et al. 2023 [27] | Wang et al. 2018 [28] | Wang et al. 2017 [29] | Yuan et al. 2015 [30] | Zhang et al. 2024 [31] | Chaoju et al. 2020 [36] | Kim et. al. 2018 [33] | Azizkhani et al. 2017 [35] | Shen et al. 2022 [34] | Cao et al. 2010 [32] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Did the research questions and inclusion criteria for the review include the components of PICO? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the report of the review contain an explicit statement that the review methods were established prior to the conduct of the review and did the report justify any significant deviations from the protocol? | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors explain their selection of the study designs for inclusion in the review? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors use a comprehensive literature search strategy? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors perform study selection in duplicate? | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors perform data extraction in duplicate? | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| Did the review authors provide a list of excluded studies and justify the exclusions? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Did the review authors describe the included studies in adequate detail? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors report on the sources of funding for the studies included in the review? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| If meta-analysis was performed, did the review authors use appropriate methods for statistical combination of results? | NA | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| If meta-analysis was performed, did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? | NA | 0 | 0 | 1 | NA | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors account for RoB in primary studies when interpreting/discussing the results of the review? | 1 | 0 | 0 | 1 | NA | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 |
| Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 |
| Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review? | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Score | 8 | 9 | 6 | 12 | 5 | 8 | 9 | 10 | 12 | 11 | 8 | 9 | 7 | 9 | 8 | 9 | 12 | 12 | 12 | 14 | 13 |
Each included study was assessed using the GRADE criteria, which provided an evaluation of the certainty of the evidence across the key outcomes. The results of these assessments are presented in (Table 3), highlighting the level of confidence we can place in the observed effects of cupping therapy in each of the included studies.
Table 3
Detail of evidence quality of pain-related outcomes
| Grade | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Disease | Intervention vs. comparison | Outcomes | risk of bias | inconsistency | indirectness | imprecision | publication bias | large effect | plausible confounding | dose response relationship | Overall |
| Cramer et al. 2020 [19] | chronic pain | cupping vs. no treatment | pain intensity | serious | not serious | not serious | not serious | not serious | no | no | no | moderate |
| Moura et al. 2018 [18] | chronic back pain | cupping therapy vs. one or more of the following groups: sham, active treatment, waiting list, standard medical treatment, or no treatment | pain intensive score | serious | not serious | not serious | not serious | not reported | no | no | no | moderate |
| Wang et al. 2018 [28] | knee osteoarthritis | dry cupping therapy + western medicine vs. western medicine | VAS scores | not serious | not serious | not serious | serious | not applicable | no | no | no | moderate |
| Li et al. | knee osteoarthritis | dry cupping therapy + western medicine vs. western medicine | WOMAC-pain | serious | not serious | not serious | serious | not applicable | no | no | no | low |
| 2017 [24] | response rate | serious | not serious | not serious | serious | not applicable | no | no | no | low | ||
| Wood et al. 2020 [22] | musculoskeletal pain (nonspecific neck pain) | dry cupping vs. no treatment | VAS | not serious | serious | not serious | not serious | not applicable | no | no | no | low |
| musculoskeletal pain (low back pain) | dry cupping vs. comparative or control group | VAS | not serious | not serious | not serious | not serious | not applicable | no | no | no | moderate | |
| low back pain | cupping vs. medication or | VAS | serious | serious | not serious | serious | not applicable | no | no | no | very low | |
| Wang et al. 2017 [29] | usual care | ODI | serious | serious | not serious | serious | not applicable | no | no | no | very low | |
| MPPI | not serious | serious | not serious | serious | not applicable | no | no | no | low | |||
| Azizkhani et al. 2018 [35] | non-specific neck pain | cupping therapy vs. other or no treatment | VAS | serious | not serious | not serious | not serious | not applicable | no | no | no | moderate |
| neck pain | cupping vs. no treatment | VAS | serious | not serious | not serious | serious | not applicable | no | no | no | low | |
| Kim et al. 2018 [33] | cupping vs. active control | VAS | serious | serious | serious | not serious | not applicable | no | no | no | low | |
| cupping plus active control vs. active control alone | VAS | serious | not serious | serious | not serious | not applicable | no | no | no | low | ||
| Cao et al. 2010 [32] | fibromyalgia | cupping plus acupuncture | VAS | not serious | not serious | serious | serious | not applicable | no | no | no | low |
| Yuan et al. 2015 [30] | chronic neck pain | cupping vs. waitlist | VAS | not serious | not serious | not serious | serious | not applicable | no | no | no | moderate |
| chronic low back cupping vs. medications pain | VAS | not serious | serious | serious | not serious | not applicable | no | no | no | low | ||
| Shen et al. | low back pain | dry cupping vs. non-cupping group | VAS | serious | not serious | not serious | serious | not applicable | no | no | no | low |
| 2022 [34] | wet cupping vs. non-cupping group | VAS | serious | not serious | not serious | serious | not applicable | no | no | no | low | |
| Chaoju et al. 2022 [36] | non-specific low back pain | blood pricking and cupping vs. other treatments | VAS | not serious | not serious | not serious | not serious | serious | no | yes | no | high |
| Bridgett et al. 2017 [17] | perceptions of pain, discomfort, physical function, physical or mental performance measures, recovery related measures, physiologic measures of stress, inflammation, or injury | cupping vs. no treatment, placebo, conventional medication, or any other intervention | VAS | serious | not applicable | not serious | not applicable | not applicable | no | no | no | very low |
| Cao et al. 2014 [17] | pain-related conditions (herpes zoster, low back pain, cancer pain, brachialgia paraesthetica nocturna, acute trigeminal neuralgia, headache, postapoplectic shoulder-hand syndrome, carpal tunnel syndrome, neck pain, osteoarthritis, shoulder pain, scapulohumeral periathritis, and ankle sprain) | wet cupping vs. no ttt | VAS | serious | not applicable | not serious | not serious | not applicable | yes | no | no | moderate |
| dry cupping vs. no ttt | VAS | serious | not serious | not serious | not serious | not applicable | no | no | no | low | ||
| Kim et al. 2011 [20] | low back pain, cancer pain, trigeminal neuralgia, brachialgia paraesthetica nocturna (bpn) and herpes zoster | cupping vs. analgesics, usual care, physiotherapies, psychological care, musicotherapy, heat pad | VAS | not serious | not applicable | serious | not applicable | not applicable | no | no | no | very low |
| Seo et al. 2021 [21] | migraine | cupping vs. placebo or conventional drug therapy | total effective rate | serious | not serious | not serious | not serious | not applicable | no | no | no | low |
| Zhang et al. 2017 [23] | cervical spondylosis, knee OA, LCFN, lumbar disk herniation, scapulohumeral periarthritis, muscle fibrositis, soft tissue contusion, acute lumbar sprain, fibromyalgia, acute ankle sprain | cupping therapy vs. acupuncture | VAS | serious | serious | not serious | serious | not applicable | no | no | no | very low |
| Ma et al. 2018 [25] | ankylosing spondylitis | cupping therapy vs. sham cupping device/placebo or western medicine | response rate | serious | not serious | not serious | not serious | not applicable | no | no | no | moderate |
| BASDAI | serious | not serious | not serious | serious | not applicable | no | no | no | low | |||
| Mohamed et al. 2023 [26] | musculoskeletal and sports conditions (including musculoskeletal dysfunction, sports injuries, low back pain, cervical pain, neck pain, plantar fasciitis, stiffness of soft tissues, fibromyalgia, myofascial pain syndrome, osteoarthritis muscle fatigue or muscle soreness) | cupping vs. usual care, no treatment | VAS | not serious | not applicable | serious | not applicable | not applicable | no | no | no | very low |
| Salazar-Méndez et al. 2023 [27] | fibromyalgia | cupping vs. acupuncture | VAS | not serious | serious | not serious | serious | not applicable | no | no | no | low |
| Zhang et al. 2024 [31] | low back pain | cupping vs. medication, usual care, sham cupping | VAS, PPI, NRS | not serious | serious | not serious | not serious | serious | yes | no | no | moderate |
Synthesis of results
Two systematic reviews and meta-analyses compared the effectiveness of cupping therapy with other interventions like conventional drugs, heat therapy, and acupuncture [17, 23]. Cao et al. [17] concluded, based on the low-quality studies, that there is moderate evidence that cupping is better than heat therapy, usual care, and conventional medications to reduce pain shortterm in patients with complaints of chronic neck pain, non-specific low back pain, osteoarthritis, carpal tunnel syndrome, acute ankle sprain, and headache. The certainty of evidence was moderate for wet cupping versus no treatment and low for dry cupping versus no treatment. When comparing cupping with acupuncture, Zhang et al. [23] concluded that there is limited evidence showing that cupping therapy and acupuncture have similar effects on relieving pain and improving other symptoms of pain related to cervical spondylosis, knee OA, LFCN, lumbar disk herniation, scapulohumeral periarthritis, muscle fibrositis, soft tissue contusion, acute lumbar sprain, fibromyalgia, and acute ankle sprain. The remaining reviews assessed the effectiveness of cupping therapy with no treatment, and the certainty of evidence was very low.
Four reviews reporting the results of RCTs for neck pain concluded that cupping might be an option to decrease neck pain and increase function [2, 3, 33, 35]. Wood et al. [22] reached a similar conclusion about using cupping for chronic neck pain compared with no treatment based on a review of fair-quality RCTs. Kim et al. [33] demonstrated that cupping reduced neck pain in patients compared with no intervention or active control groups, or as an add-on treatment. Depending on the type of control group, cupping was also associated with significant improvement in terms of function and quality of life, with the certainty of evidence being low. Additionally, Azizkhani et al. [35] provided some evidence that cupping therapy may improve the treatment of patients with neck pain with a certainty of evidence of moderate.
The conclusion of seven reviews [18, 19, 22, 29, 31, 34, 36] assessing the effectiveness of cupping for nonspecific low back pain suggested that cupping was more effective than no treatment to reduce pain. Wood et al. [22] also concluded that there is low to moderate evidence that cupping is superior to no-treatment to relieve pain in patients with chronic lower back pain. Evidence suggests that cupping is better than no treatment to decrease pain in the short term for patients with knee OA and fibromyalgia [24, 27, 28, 32]. However, according to Cramer et al. [19], the evidence is limited. The authors also concluded that the evidence supporting the effectiveness of cupping therapy for carpal tunnel syndrome is limited, and the certainty of evidence was moderate. Wang et al. [29] concluded that cupping therapy may be a promising and safe therapy method for subacute or chronic low back pain. Cupping therapy can significantly decrease the VAS scores and ODI scores compared to the control management (usual care/medication). High heterogeneity and risk of bias existing in trials limited the authenticity of the findings and the certainty of evidence was very low for VAS and ODI and low for MPPI.
Additionally, Zhang et al. [31] concluded that high-to moderate-quality evidence indicates that cupping significantly improves pain and disability. The effectiveness of cupping for LBP varies based on treatment durations, cupping types, treatment locations, and LBP classifications. Cupping demonstrated a superior and sustained effect on pain reduction compared with medication and usual care, and the certainty of evidence was moderate. Chaoju et al. [36] also revealed that blood pricking and cupping therapy can safely and effectively reduce pain and improve functional impairment in patients with NLBP, and the certainty of evidence was high. Shen et al. [34] concluded that wet cupping therapy effectively reduces the pain intensity of LBP. Furthermore, both dry-wet cupping therapies improved the quality of life in patients with LBP, and the certainty of the evidence was low.
Yuan et al. [30] performed a study to review and analyse the existing data about pain and disability in Traditional Chinese medicine treatments including cupping for both neck pain and low back pain. They demonstrated that acupuncture, acupressure, and cupping could be efficacious in treating pain and disability for chronic neck pain or chronic lower back pain in the immediate term. The certainty of evidence was moderate for neck pain and low for low back pain.
Two systematic reviews targeting musculoskeletal and sports conditions in athletes concluded that the current evidence prevents recommending in favour or against cupping therapy to decrease perceived pain, disability, and exertion after training. Wood et al. [22] obtained a similar conclusion when analysing the effectiveness of cupping to improve the range of motion by improving the flexibility of the hamstrings and iliotibial band with the certainty of evidence was low for neck pain and moderate for low back pain. However, Mohamed et al. [26] concluded that cupping therapy has low to moderate evidence for musculoskeletal and sports rehabilitation and might be used as a useful intervention because it decreases the pain level and improves blood flow to the affected area with low adverse effects and the certainty of the evidence was very low.
Two systematic reviews evaluated the efficacy and safety of cupping therapy for treating patients with KOA. The findings of Li et al. [24] and Wang et al. [28] both demonstrate that only weak evidence supports the hypothesis that cupping therapy can effectively improve treatment efficacy and physical functions in patients with KOA, and the certainty of evidence was low for Li et al. [24] and moderate for Wang et al. [28].
Single systematic reviews concluded that cupping therapy is potentially effective compared with no intervention to decrease pain due to headaches [21] and the certainty of evidence was low, trigeminal neuralgia [20] and the certainty of evidence was very low, and shoulder pain [22] and ankylosing spondylitis [25] and the certainty of evidence was moderate for response rate and low for BASADI. Additionally, Salazar-Méndez et al. [27] conducted a review to evaluate the efficacy of cupping therapy on pain, quality of life, sleep disorders, and the impact of the disease in subjects with fibromyalgia. It concluded that there is a discrepancy in the efficacy of cupping therapy in improving pain intensity, quality of life, sleep disturbances, and disease impact in individuals with fibromyalgia, and the certainty of evidence was low [27]. Also, Cao et al. [32] conducted a systematic review of the beneficial and harmful effects of TCM therapies for FM, concluding that TCM therapies appear to be effective for treating FM with a certainty of evidence as low.
Cupping therapy adverse events
Five systematic reviews [21, 27, 29-31] did not specify the investigation of adverse events, harms, or side effects for cupping therapy, and another review [20] reported that none of the included studies presented information on side effects. One review [22] reported no severe adverse events without presenting the types of events. The remaining reviews found that cupping therapy can cause mild or moderate events [17, 23], hematoma [24, 28], pain at the site of application, increase in pain or tingling [19], dizziness [22], and that occurrence of adverse events was superior for cupping therapy than for no-treatment or other active interventions [18]. While one review reported adverse outcomes like nausea and vomiting, abdominal pain, and diarrhoea when combined with Western medical therapies [25]. Circulatory instability in the first minute after treatment, tension headaches, migraine attacks, reappearing tinnitus, and wound healing were all detected in one review [26].
Discussion
This umbrella review aimed to synthesise systematic reviews investigating the effectiveness of cupping therapy for musculoskeletal pain in athletes and the general population. The findings from this umbrella review suggest that cupping therapy may be more effective than passive interventions such as heat therapy, usual care, conventional medications, and no treatment. However, most of the systematic reviews included in this analysis revealed that cupping therapy is generally ineffective in improving musculoskeletal pain in athletes and the general population. However, when compared to acupuncture, the effects were found to be similar. As far as recommending cupping therapy for athletes, there is not enough evidence to support it. Moreover, the results of most of these studies displayed shallow confidence. There are some risks associated with cupping therapy, such as hematoma, pain at the site of application, increased pain or tingling sensations, and dizziness.
The effectiveness of cupping therapy in relieving pain varies depending on the type of intervention being compared. These findings come from a recent meta-analysis that reported that cupping therapy is more effective than standard medical care in treating low back pain [30]. They found that four sessions of cupping therapy significantly decreased pain and increased straight-leg raises, lumbar flexion ROM, and the painpressure threshold. Cupping therapy can be used alone or with other rehabilitative or pharmaceutical interventions in treating cervical or lower back pain [37]. Cupping therapy can reduce pain and muscle tenderness and improve ROM in patients with sub-acute or chronic lower back pain. The analysis of the six studies included in Mohamed et al. [26] revealed that the evidence supporting the effectiveness of cupping therapy in treating low back pain is of low to moderate quality.
Cupping therapy was found to be more effective than passive interventions such as heat therapy, usual care, conventional medications, and no treatment. This aligns with the reported findings of a systematic review and meta-analysis [12, 37], which found significant short-term effects of cupping on pain intensity compared to no treatment. The results from two previous cupping overviews [12, 37] showed that cupping effectively reduced pain in mixed pain conditions. However, the authors clarified that these findings were from low-quality trials, and no firm recommendations were able to be made. Unfortunately, many interventions reach the patients before being adequately tested in clinical trials with proof of effectiveness and safety [10, 13, 38]. When cupping therapy was compared to acupuncture, the effects were similar. This finding is consistent with Cramer et al., who found no significant effects compared to sham cupping or other active treatments. This suggests that cupping therapy could serve as an alternative to acupuncture for some patients [17].
Regarding the application of cupping therapy in athletes, the review found insufficient evidence to support its use. Similarly, the latest research shows that pre-exercise dry and wet cupping therapies do not positively impact anaerobic performance and related physiological responses [39]. Anaerobic performance is crucial for power and team sports such as soccer, football, sprinting, speed skating, basketball, and lacrosse. As a result, coaches and practitioners working with powerful athletes or teams are advised against using cupping therapy before sporting events. Our review also revealed no adverse effects from cupping therapy on athletes, so athletes can continue using it if it is part of their routine or if they believe it provides ergogenic benefits. This highlights the need for more high-quality research before any definitive recommendations can be made.
However, in the general population, the review identified some minor risks associated with cupping therapy. These include hematoma, pain at the application site, increased pain or tingling sensation, and dizziness. Other recent studies have reported some of these risks [26]. These potential risks highlight the importance of considering individual patient characteristics and using a careful, patient-centred approach when considering cupping therapy [26, 40].
Limitations of the study
The results of most of these studies displayed shallow confidence. This significant limitation suggests that the findings should be interpreted with caution. Further determining the necessity of using a placebo from a scientific point of view is challenging. The widely studied psychosomatic placebo effect significantly undermines its importance as the gold standard in clinical trials. Hence, high-quality studies are needed to increase confidence in these findings.
Practical implications
Based on the systematic reviews provided, cupping therapy is a potential treatment for conditions such as chronic neck pain, non-specific low back pain, osteoarthritis, carpal tunnel syndrome, acute ankle sprain, and headache. It has shown better results than heat therapy, usual care, and conventional medications, and similar effects to acupuncture. However, the overall confidence in these results is low due to methodological issues in the reviews, indicating a need for further high-quality research. For athletes, the evidence is currently insufficient to recommend cupping therapy for reducing perceived pain, disability, and exertion after training. While cupping therapy can cause mild or moderate adverse events, no serious events were reported. Therefore, while cupping therapy shows promise, healthcare providers and patients should consider the potential benefits, risks, and quality of the evidence when considering it as a treatment option. Individual patient characteristics and preferences should always be considered in clinical decision-making.
Conclusions
There is insufficient confidence in cupping therapy for musculoskeletal conditions, as the current evidence does not support its efficacy. Large, rigorously designed randomised controlled trials (RCTs) are needed to investigate the effectiveness of cupping therapy. Utilising unproven therapies that, at best, offer a placebo effect is ethically questionable. Furthermore, besides the lack of positive effects, we cannot disregard the potential for unknown adverse effects. Therefore, physiotherapists, coaches, and trainers must consider these findings when evaluating cupping therapy for musculoskeletal pain.
Direction for future studies
This review provides some exciting insights into the potential effectiveness of cupping therapy for musculoskeletal pain. The low confidence in the results and the identified risks underscore the need for further research in this area. Future studies must be well-designed and adequately powered to provide more definitive answers. This will help further our understanding of the effectiveness and safety of cupping therapy for musculoskeletal pain in athletes and the general population.