Introduction
Lumbar instability (LI), a subcategory of mechanical low back pain (LBP), has been extensively studied by many researchers with a particular focus on its management strategy [1-6]. In Thailand, the prevalence of chronic LBP (CLBP) with LI is approximately 54.54% among patients with CLBP [2, 3, 5]. Notably, previous research undertaken with 694 young adults (aged 20-39 years) with CLBP, found 319 individuals had LI [2]. Sedentary individuals who spend prolonged periods in the sitting posture result in trunk muscle fatigue due to the continuous contraction of the deep trunk muscles, along with an increase in lumbar repositioning error (LRPE) [7-9]. Deep trunk muscle fatigue and errors in lumbar positioning sense may reduce the muscular support to the spine, leading to impairment of motor coordination, reduced intervertebral disc height, and a diminished ability to perceive and control the precise position of the lumbar spine [7-9]. Therefore, prolonged sitting postures may affect lumbar stability and ultimately lead to LBP [7-9]. Lumbar stabilisation exercises (LSEs) are proposed to improve lumbar stability and enhance trunk muscle coordination and are recommended as therapeutic exercises for patients with LI [4, 6, 10]. Abdominal muscle activation techniques have been used as a training method to improve lumbar stability [11-15]. The abdominal drawing-in manoeuvre (ADIM) and abdominal bracing (AB) techniques are two popular techniques that emphasise enhancing abdominal function [11-15]. The ADIM is recommended for preferential activation of the transversus abdominis (TrA) muscle while minimising the activation of superficial muscles, such as the rectus abdominis (RA) and abdominal external oblique (EO) muscles [11-15]. Conversely, AB involves the contraction of all the anterolateral abdominal muscles [11-15]. Consequently, the key difference between the techniques is the targeted muscle activation [11-15].
The use of digital health to administer treatment offers many benefits to the clinician and patients. A basic telerehabilitation system includes at least one camera, allowing a physical therapist to see the patient and directly monitor the therapy through videoconferencing [16]. Patients are provided with an opportunity to be independent, gain personal control, and make decisions in the management of their condition [17-19]. Physical therapists could conveniently deliver healthcare services to patients in the comfort of their homes, thereby eliminating the issue of distance between physical therapists and patients [17]. Telerehabilitation reduces the cost, minimises travel time, and provides access to care for individuals in remote areas or those facing physical limitations, transportation difficulties, and socioeconomic barriers [16-18]. Moreover, the use of telerehabilitation is especially important during epidemics and has significant potential in modern therapy [20-21].
Based on the hypothesis, the ADIM technique is more likely to activate the TrA muscle, which is used to stabilise the lumbar spine, and may be more beneficial for LI compared to the AB technique. To date, no studies have directly compared the effects of these two abdominal muscle activation techniques via telerehabilitation in participants with CLBP and LI. The purpose of the current study was to investigate the effects of two different LSE techniques (ADIM and AB) delivered via telerehabilitation on LRPE, pain scores, and TrA muscle performance in seated sedentary patients with CLBP and LI. The findings will provide practical implications and recommendations for the LSE technique using a telerehabilitation approach to improve outcomes for participants with CLBP and LI.
Material and methods
Study design
The study was a parallel-group, randomised, controlled trial conducted (between May 2023 and January 2024) at the research laboratory of the Faculty of Physical Therapy, Srinakharinwirot University, Thailand.
Participants
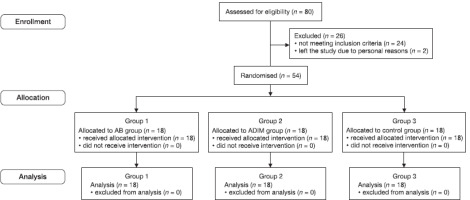
All participants provided written informed consent before the study protocol began. The sample size was calculated using the G*Power program (G*Power version 3.1.9.6, University of Kiel, Germany). The calculation considered the mean of LRPE between groups (from a pilot study), with an alpha of 0.05, power (1-β) of 80%, effect size of 0.52, and a 30% attrition rate. Eighteen participants per group were required, with a total of 54 participants for the current study. Eighty participants with CLBP were recruited through purposive sampling via electronic posters on social media platforms. Participants were included if they were aged 18-39 years with CLBP, defined as pain between T12 and the gluteal fold, with mild to moderate pain levels (NRS scores 3-7) present for at least 3 months. CLBP with LI scored at least 7/14 on the Thai version of the LI screening questionnaire; a normal body mass index (BMI = 18.5-25 kg/m2), and a sedentary lifestyle (sitting for more than 2 hours per day) [7, 9, 22]. Participants were defined to have LI by the principal researcher, a physical therapist with 9 years of experience, based on the Thai version of the LI screening questionnaire [2, 23]. The questionnaire includes 14 items related to the patient’s feelings, behaviour, activity and position adopted, with scores ranging from 0 (not related to having LI) to 14 (strongly related to having LI). Participants with neurological deficits, spine pathology (e.g., spinal deformities, history of trauma, or surgery in the lower back region), or who were pregnant were excluded from the study [2, 9, 24, 25].
This study was conducted following the flowchart displayed in Figure 1. The information and procedures of the study were explained to the eligible participants, and they were asked to sign an informed consent form before participating. At the first visit, all participants were initially screened through an interview and physical examination by a physical therapist who was the principal researcher. Age, weight, height, BMI, and LI score were collected. Then, the baseline outcomes of the participants were assessed, including LRPE, NRS, and TrA muscle performance.
All participants were randomly allocated to either the AB group (group 1), ADIM group (group 2), or control group (group 3) by the research assistant. Random numbers were computer-generated in block sizes of three and six and kept in sealed envelopes with consecutive numbering. The principal researcher was blinded to the treatment allocation group. The participants were familiarised with the group protocol to which they were assigned in the research laboratory. After 4 weeks of treatment, all participants were asked to stop their treatment completely. The outcomes were remeasured 4 weeks after starting the treatment programs.
Interventions
Group 2
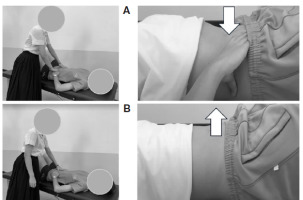
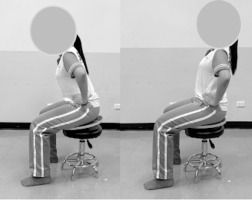
For the ADIM technique, the participants were instructed to slowly and gently draw the abdominal wall inward, maintaining the lumbar spine in a neutral position, as in Figure 3 [11-15].
Figure 3
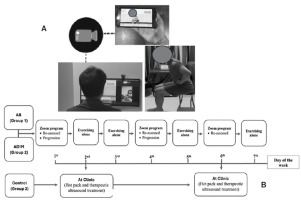
(A) An example of telerehabilitation via a Zoom program, (B) The weekly intervention process across the three groups
Group 3
Participants in the control group received a hot pack and therapeutic ultrasound, which are standard treatments for the management of LBP in Thailand [25]. Participants received 5 minutes of therapeutic ultrasound at a 1-MHz frequency with an intensity of 0.8-1.0 W/cm2 on continuous mode. Then, they received 15 minutes of heat via a hot pack, applied to the lower back in a prone lying position [25].
Experimental protocol
The participants were invited to the laboratory to practice the exercise techniques and familiarise themselves with the telerehabilitation protocol before starting 4 weeks of LSE. The participants were instructed to hold the abdominal muscle contraction by ADIM or AB techniques for 10 seconds while maintaining a normal breathing cycle [11-15, 24-27]. To ensure the participants performed each technique correctly, a pressure biofeedback device (Chattanooga Australia Pty Ltd, Brisbane, QLD, Australia) provided feedback and facilitated the correct performance during training in the crook lying position. The pressure biofeedback device was placed under the lower back with the lower edge in line with L5/S1 and inflated to 40 millimetres of mercury (mm Hg). The participants passed the performance test when the pressure gauge reading was within 40 ± 4 mm Hg [27]. Conversely, if the pressure gauge reading was outside the target range, the participant was required to practice the technique again [27]. When all participants could perform the exercise correctly, they were given an electronic book that contained illustrations and an explanation of the exercise program (Supplementary) for their home-based exercise. The exercise protocol utilised a modified version of the Saiklang et al. [22] protocol. To date, several studies have supported that 4 weeks of LSEs can reduce pain and improve trunk muscle performance, which are common issues in patients with LI [17, 18, 25, 28]. This study also included a 4-week LSE program. The LSE program consisted of 10-second holds with 10 repetitions/set for 10 sets/day. The LSE program progressed from supine to sitting positions. Their performance was monitored via video conferencing for 4 consecutive weeks. The 4-week LSE program consisted of two stages. In the first stage (weeks 1-2), the treatment focused on isolating low-load activation of the abdominal muscles. Subsequent training involved activating these muscles under low-load conditions. In the first week, to activate the abdominal muscles, the participants were positioned lying on a bed. In the second week, abdominal muscles were activated with controlled movements of the lower extremities in the supine position. The participants were asked to place their hands on the upper part of their iliac crests and contract their abdominal muscles until they felt a contraction beneath their hands. The second stage (weeks 3-4) emphasised increasing the accuracy and duration of the exercises. Abdominal muscle activation with controlled spinal movements was performed and progressed to high-load positions. In the third week, abdominal muscles were activated while sitting with and without a balance board. In the fourth week of the exercise program, a combination of supported dynamic lumbar extension exercises was performed in the sitting position. All participants were asked to record details of their exercise practice on a Google Sheet application throughout the study period to monitor their compliance. Additionally, the researcher made phone calls to all participants to encourage them to continue their home exercises during the study period.
The conditioning procedure for 1 week is representative of the remaining 3 weeks in the 4-week process, as shown in Figure 3. The participants in the control group (group 3) received treatment sessions that lasted 20 minutes and were administered twice per week (on the 2nd and 6th days) for 4 weeks by a physical therapist at a physical therapy clinic. The participants in the AB (group 1) and ADIM (group 2) groups performed the exercise program via an interactive device for 30 minutes per session, 3 times per week (on the 1st, 4th, and 6th day) for 4 weeks, using the Zoom program. Participants were also asked to perform the exercise by themselves, 4 times per week (on the 2nd, 3rd, 5th, and 7th day) for 4 weeks.
The exercise performance was re-assessed via telerehabilitation supervision (on the 1st and 4th day) at each session to determine whether the participants could correctly perform the exercises, as shown in Figure 3. As the exercise program was designed as a milestone, participants would progressively change into a new position once a week. The criteria for progressing to the next position was when the participant could sustain the ADIM or AB for 10 seconds and complete 10 repetitions of the exercises in the current position. If participants experienced pain or did not perform the exercises adequately, they were not allowed to proceed to the next position and were instructed to continue training in the current position. However, if they had no pain and successfully performed the current position, they progressed to the next exercise position [22, 24, 25]. The progress of the exercise positions is detailed in the supplementary material.
Lumbar repositioning error test
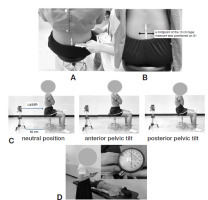
The primary outcome is the LRPE test, as in Figure 4. To test the LRPE [9, 24, 25], participants were asked to sit in an adjustable chair and instructed to maintain a sitting posture with their hips, knees, and ankles at 90 degrees. Their feet were supported, arms crossed on their chest, and their lumbar spine held in a neutral position. The pelvis and lumbar spine were manually positioned into an upright neutral position by aligning the inferomedial aspect of the anterosuperior iliac spine (ASIS) and the posterosuperior iliac spine (PSIS) using a palpation meter with a spirit level. A 10-centimetre tape measure with millimetre markings was placed on the first sacral spine (S1) as the starting point. A laser lever device was positioned directly on the start point of the marked line. Participants were instructed to remember the neutral position and then move their pelvis twice, from maximum anterior to maximum posterior tilt, holding each position for approximately 5 seconds before returning to the neutral position. Participants were allowed to practice the repositioning test twice before the actual test commenced. The procedure was performed 3 times, with one-minute rest intervals, and the average values of the measurements were used for analysis [9, 24, 25]. The researcher observed the correct movement of the pelvis during the measurement process. Deviance from the start point was measured in centimetres as LRPE. The value of LRPE was calculated as an absolute error (AE), which represents error magnitude and is the most used measure. AE is the unsigned difference from the start point [9, 24, 25].
Figure 4
The LRPE testing:
(A) The pelvis and lumbar spine were manually aligned using a palpation meter
(B) A midpoint of the 10 cm tape measure was positioned on S1
(C) A laser pointer was kept at a distance of 50 cm behind the participant and pointed at S1 as the starting point of the marked line. The participant performed a neutral position, anterior pelvic tilt and posterior pelvic tilt
(D) The pressure biofeedback device was placed under the lower abdomen, with its lower edge aligned with the anterior superior iliac spine and inflated to 70 mm Hg
Pain intensity
Pain intensity was assessed using the 11-point NRS (0-10 NRS). Subjective measures of pain were obtained from the NRS, which was used to assess pain over a 24-hour period on a scale ranging from 0 “no pain” to 10 “worst possible pain”. Boonstra et al. [29] reported that NRS scores of < 5 correspond to mild pain intensity, scores of 6-7 correspond to moderate pain intensity, and scores of > 8 correspond to severe pain. The minimum clinically important change (MCIC) for pain on the NRS is reported to be at least 2.5 points for people with CLBP [7].
Transversus abdominis muscle performance
The ability to contract the TrA muscle performance was assessed using a clinical muscle test (prone test with the pressure biofeedback unit). The pressure biofeedback device was placed under the lower abdomen, with the lower edge aligned with the ASIS and inflated to 70 mm Hg. The results of the TrA muscle performance test were recorded based on the change in pressure (either an increase or decrease in mm Hg) measured by the device [6, 22, 24, 25]. A TrA muscle contraction that resulted in an increase in mm Hg was classified as a ‘poor’ contraction. A reduction in pressure by approximately 0-2 mm Hg, in the absence of spinal or pelvic movement and without bulging of the abdomen, was classified as a ‘fair’ contraction, while a reduction of 3-6 mm Hg was classified as a ‘good’ contraction [26].
Statistical analysis
Prior to statistical analysis, values for LRPE, NRS, and TrA muscle performance were assessed for normal distribution using the Kolmogorov-Smirnov test, which confirmed the assumption of normal distribution (p > 0.05). A one-way ANOVA was employed to examine the differences in LRPE between groups. Differences in LRPE within groups were assessed using dependent sample t-tests. Differences in NRS and TrA muscle performance within groups for non-normally distributed data were analysed using the Wilcoxon signed-rank test. Differences in NRS and TrA muscle performance between groups were analysed using the Kruskal-Wallis test. A significance level ofp < 0.05 was used for all statistical evaluations. Data analysis was conducted using SPSS software version 26.0 (IBM SPSS Statistics, SPSS Inc., Chicago, IL, USA).
Results
The demographic data of all participants are presented in Table 1. There were no significant differences in demographic characteristics between the groups (p > 0.05). All participants completed the 4-week program. The participants reported no adverse effects and were able to maintain their condition throughout the program.
Table 1
Baseline characteristics of the participants (n = 54)
In the control group, the LRPE remained unchanged after the 4 weeks of treatment (p = 0.220, Table 2). However, in the AB and ADIM groups, there was a significant decrease in LRPE after 4 weeks of exercise (AB, p = 0.001 and ADIM, p = 0.001). When comparing between groups, the ADIM group exhibited a significantly lower LRPE compared to the control group after the 4 weeks of treatment (p = 0.014); however, there was no significant difference with the AB group.
Table 2
The results of absolute lumbar repositioning error before and after 4 weeks of the program (n = 54)
Within-group comparisons showed a significant reduction in pain intensity after 4 weeks of treatment in the AB (p = 0.001), ADIM (p = 0.001), and control (p = 0.001) groups (Table 3). However, when comparing between groups, none of the groups reported a significant change in NRS after the 4 weeks of treatment.
Table 3
The results of pain score before and after 4 weeks of the program (n = 54)
Within-group comparisons showed a significant improvement in TrA muscle performance, as measured by the pressure biofeedback device, after the 4 weeks of treatment in the ADIM (p = 0.001) and AB groups (p = 0.033, Table 4). When comparing between groups, the AB group showed a significant improvement in TrA performance compared to the control group (p = 0.027). The ADIM group exhibited a significant improvement in TrA muscle performance compared to the control (p < 0.001) and AB groups (p < 0.001) after 4 weeks of treatment.
Table 4
The results of TrA muscle performance before and after 4 weeks of the program (n= 54)
Discussion
The results indicated that 4 weeks of LSE using ADIM and AB techniques via telerehabilitation can improve LRPE, NRS, and TrA muscle performance. However, the ADIM technique led to the most significant improvement in TrA muscle performance and LRPE. A previous systematic review and meta-analysis analysed the effectiveness of real-time telerehabilitation compared to standard in-person practice in patients with musculoskeletal disorders. They demonstrated that telerehabilitation is equally effective as in-person rehabilitation in improving physical function, disability, and pain [30]. Moreover, Akodu et al. [17] reported that telerehabilitation-based LSE was as efficacious as clinical-based LSE in decreasing pain-related disability and improving pain self-efficacy. Additionally, Karaduman et al. [18] found that tele-supervised LSE was more beneficial, showing significant improvements in functionality and pain compared to unsupervised LSE, highlighting its safe and effective use in patients with non-specific CLBP.
To the best of our knowledge, the current study is the first study that investigated the effects of LSE using ADIM and AB techniques via telerehabilitation in individuals with CLBP and LI. Although all three groups showed a statistically significant reduction in pain after 4 weeks of intervention, the AB and ADIM groups had a clinically significant reduction in pain intensity (> 2.5 points) [7]. The results of this study indicated that LRPE can be restored after 4 weeks from LSE within the ADIM (p = 0.001) and AB (p = 0.001) groups when compared to baseline. Notably, the ADIM group exhibited a significantly lower LRPE compared to the control group after 4 weeks of treatment (p = 0.014). This result aligns with previous studies by Puntumetakul et al. and Yalfani et al. [31], which reported that LSE can improve the accuracy ofjoint position sense in patients with LBP. The present study also reported that 4 weeks of LSE can improve TrA muscle performance in ADIM (67 mm Hg) and AB (70 mm Hg) groups. Hides et al. recommended that a reduction in pressure by approximately 0-2 mm Hg be classified as a ‘fair’ contraction, while a reduction of 3-6 mm Hg be classified as a ‘good’ contraction. An increase in deep trunk muscle activity stimulates muscle spindles and joint receptors, enhancing the accuracy of the sensory integration process and enabling correct lumbar joint repositioning [24, 25, 32]. Additionally, pain is associated with decreased proprioception and muscle strength, which affects sensory information and compromises the relationship between postural responses and sensory information [24, 25, 32]. Therefore, improvement in LBP and TrA muscle performance after 4 weeks of LSE can enhance proprioception.
The LSE using the ADIM technique led to greater improvement in TrA muscle performance compared to the AB group. This improvement might be attributed to the specific training effect of LSE, which focuses on preferentially retraining the TrA muscle [11-15]. Saiklang et al. [33] demonstrated that providing participants with instructions on co-contraction of the deep trunk muscles (ADIM technique) during sitting can increase trunk muscle activity, except for the RA muscle. Previous studies demonstrated that the ADIM and AB techniques activate different target trunk muscles [11-15]. Oshikawa et al. [13] examined the electromyography (EMG) activity of the TrA, abdominal, internal oblique (IO), abdominal EO, and RA muscles during AB and ADIM techniques in six different positions. TrA activity was higher in the standing position than in the prone and side-lying positions using the ADIM technique. IO and EO activities were higher during ADIM than AB. Moreover, RA showed higher activity during AB than ADIM. In the same way, TrA thickness was significantly greater during ADIM than during AB in the supine and sitting positions [12]. Moreover, Tsao et al. [34] reported that ADIM, which involves isolated voluntary contractions of the TrA muscle, has been associated with neural reorganisation in the motor cortex, potentially reducing the recurrence of pain by improving neural control over spinal stability. This indicates that the benefits of ADIM may not be only mechanical but also neuromuscular, enhancing the body’s internal coordination and control mechanisms [34]. Therefore, the ADIM technique may be more effective than the AB technique.
Thermal therapy treatment for patients with CLBP and LI can reduce LBP pain rating scores, but it may not be sufficient for improving trunk muscle performance and lumbar joint proprioception. Physical therapists should consider LSE for these additional benefits. LSE aims to improve neuromuscular control skills, relearn normal functions, and enhance the endurance of the trunk muscle system around the lumbar spine to maintain static and dynamic spinal stability [4, 6, 22, 24, 25, 31]. The TrA muscle’s role is considered critical in providing a stiffening effect on the lumbar spine through its attachment to the thoracolumbar fascia, resulting in spinal stability in patients with CLBP with LI [3, 4, 6]. For clinical practitioners, this study’s findings provide additional knowledge and understanding of LSE using ADIM and AB techniques via telerehabilitation for CLBP with LI. The ADIM technique produced a noticeable improvement in the TrA muscle performance, the key muscle contributing to the stability of the lower back region. Physical therapists may consider teaching LSE via telerehabilitation to the participants using the ADIM technique, as it increases TrA muscle performance, improves LRPE, and reduces NRS scores in CLBP with LI.
There are some limitations to the current study. Firstly, the investigation involved young participants with CLBP and LI, covering only a narrow age range, which may not apply to other age groups. Secondly, digital technology may exclude older individuals [19], meaning the results of LSE via telerehabilitation may differ from those of the present study. Thirdly, TrA muscle performance was not assessed directly, such as through EMG or ultrasonographic imaging. Further studies are needed to measure the effect of this program on TrA muscle activity. Fourthly, the telerehabilitation setting limits the therapist’s ability to provide direct posture correction and muscle activation guidance which may provide less assistance to the participant during the exercise in comparison to that provided in the clinical setting. Finally, additional research is needed to investigate the follow-up effects of the program, which currently limits our understanding of its sustained benefits over time.
Conclusions
This study concludes that LSE using AB and ADIM techniques via telerehabilitation can improve LRPE, NRS, and TrA muscle performance in participants with CLBP and LI, particularly those with a sedentary lifestyle. The ADIM technique significantly enhances TrA muscle performance, which is crucial for lumbar stability. Therefore, in clinical practice, the ADIM technique has the potential to be an effective method for teaching LSE to participants with CLBP and LI.