Introduction
Stroke is predicted to afflict around one in five people in nations with high incomes, but it can impact as many as one in two people in areas with low incomes [1]. The disability-adjusted life years (DALYs) are projected to show a large increase by the year 2050, and it is anticipated that the mortality rate from stroke will have climbed by fifty per cent by that time [2]. Post-stroke motor deficits in the lower extremities frequently lead to gait abnormalities that are further exacerbated by sensory impairments, balance challenges, and motor weakness [3].
Sensory input from the feet is crucial for the transmission of information to the central nervous system, which is responsible for postural stability and equilibrium regulation. Reduced sensitivity, particularly in senior adults and those with neurological conditions, increases the likelihood of falls [4]. Fast- and slow- adapting receptors in the feet detect dynamic stimuli and static pressure, respectively; nevertheless, ageing and disease can compromise these sensory functions, underscoring the need for customised therapy to preserve foot sole sensitivity and balance [5].
Somatosensory deficiencies frequently occur poststroke, impacting over 80% of survivors, especially in proprioception and tactile sensitivity, which are essential for balance and coordinated ambulation [6]. These deficits result in uncoordinated and imprecise motions, hindering daily activities such as ambulation [7]. None- theless, sensory deficits in the lower extremities are insufficiently investigated in rehabilitation studies, constraining the efficacy of traditional gait-oriented interventions [8].
Recent research has emphasised the promise of somatosensory stimulation in motor relearning and spasticity alleviation. Nevertheless, its impact on lower limb function in stroke survivors has been underexplored. A pilot study integrating somatosensory stimulation with task-specific gait training in thirty-four individuals yielded encouraging effects. However, additional research is required to validate these findings in larger cohorts [9]. Furthermore, discomfort-inducing insoles have been employed to address gait asymmetry in unilateral deficits, but the long-term effectiveness of this method remains ambiguous [9].
Compelled body weight shift (CBWS) therapy is an innovative method aimed at redistributing weight to the affected side in stroke patients using a shoe insert that elevates the less-affected limb. The method has effectively improved static weight-bearing symmetry and increased gait velocity. However, enhancements in gait symmetry have not consistently correlated with improvements in static weight-bearing symmetry or gait velocity, as reported in the literature [10, 11]. Given the widespread challenges encountered by stroke survivors due to motor and sensory deficits, the integration of plantar somatosensory stimulation and CBWS presents a promising intervention strategy with global relevance, addressing a critical gap in stroke rehabilitation research.
This study evaluated the impact of integrating plantar somatosensory stimulation with the CBWS protocol on lower limb motor function and gait in stroke patients. We hypothesised that this integrated method would markedly improve motor function and gait metrics in stroke patients.
Material and methods
Study design
This single-blind, randomised, controlled trial was conducted at Murtala Muhammad Specialist Hospital and Aminu Kano Teaching Hospital in Kano, Nigeria. Recruitment took place from october 2023 to April 2024.
The study involved the randomisation of sixty stroke patients into four groups, including control, CBWS, textured insoles (TI), and CBWS+TI (combined). Randomisation was stratified by age, gender, and stroke type to guarantee equitable allocation, as these variables are recognised to impact prognosis. Sequentially numbered, opaque, sealed envelopes were employed to accomplish allocation concealment. outcome measures were evaluated at baseline, four weeks, and eight weeks. An assessor blinded to group assignments conducted evaluations to guarantee impartial measurement of primary and secondary outcomes at each designated time point.
Participants
Sixty individuals who had experienced a stroke were recruited from the outpatient units of Aminu Kano Teaching Hospital and Murtala Muhammad Specialist Hospital, Kano, Nigeria. The recruitment process was structured as follows: (1) initial assessment of patients based on clinical characteristics; (2) a detailed explanation of the trial aims and rehabilitation objectives by the primary researcher; and (3) obtaining informed consent, which patients provided through signing or thumb printing the consent forms.
Inclusion criteria
Participants were eligible for the study if they were 18 years or older, had experienced a stroke, and presented with residual gait impairment lasting at least three months post-stroke. Additionally, participants needed to possess the cognitive ability to understand and comply with simple instructions.
Exclusion criteria
Individuals were excluded if they had comorbid neurological conditions, such as Parkinson’s disease, or musculoskeletal issues affecting the bones or soft tissues of the lower limb that could interfere with the study protocols.
Sample size
G*Power software version 3.1 calculated the study sample size. Calculations were based on an effect size of 0.28, derived from a meta-analysis of randomised controlled trials assessing the effects of plantar somatosensory stimulation in stroke patients. With a desired power of 95% and a significance level of p = 0.05, it was determined that 48 participants would be needed to detect statistically significant differences. Considering a potential attrition rate of 20%, the total sample was set at 60 participants, allowing for 15 individuals per group across the four study groups. outcome measures
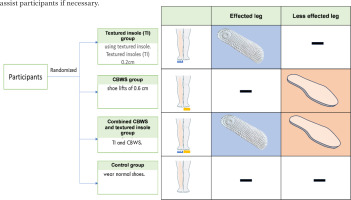
Participants in the TI group received plantar sensory stimulation through TIs sourced from commercially available slippers (Product No. 4549131140668; Daiso Sangyo (Thailand) Ltd., Bangkok, Thailand). These insoles, featuring nodules of 0.2 cm and 0.5 cm in diameter at heights ranging from 0.2 cm to 0.5 cm, were strategically placed at key areas of the foot to maximise sensory input [12] and were worn inside the participants’ shoes. The CBWS group used shoe lifts made from a medium hardness foam material, ethylene vinyl acetate, measuring 0.6 cm in height, which were inserted into the shoes of the unaffected limb. Participants in the combined group received both interventions, while those in the control group wore standard shoes without modifications (Figure 1). Throughout the eight-week intervention period, all participants were instructed to walk 2,000 steps indoors three times a week [12]. Step counts were monitored using a pedometer attached to the mid-thigh of the unaffected limb. For safety and comfort, chairs were available at both ends of the walkway for resting as needed, and the walkway was regularly cleaned and inspected before each session. A researcher was always on standby to assist participants if necessary.
Figure 1
Illustration of the experimental groups. Participants were divided into control, compelled body weight shift (CBWS), textured insoles (TI), and CBWS+TI (combined) groups. TI participants wore TIs in the affected leg, while CBWS participants used shoe lifts in the less affected leg. The Combined group received both interventions, and the control group wore standard shoes. All participants were instructed to walk 2,000 steps indoors three times a week during the eight-week intervention.
Outcome assessments were conducted by experienced physical therapists, blinded to group assignments, at baseline, four weeks, and eight weeks. Additionally, any adverse effects experienced by participants, such as headaches, pain, and dizziness, were meticulously documented during each session.
Fugl-Meyer Assessment Lower Extremity
The Fugl-Meyer Assessment Lower Extremity (FMA- LE) assesses various dimensions of motor function, including reflex activity, volitional movement within synergies, volitional movement mixing synergies, volitional movement with minimal to no synergies, and normal reflex activity. The scoring system for the FMA-LE ranges up to a maximum of 28 points, with higher scores indicating superior motor performance. This comprehensive assessment provides a detailed measure of motor recovery in individuals who have suffered a stroke [13].
Semmes-Weinstein Monofilaments
Cutaneous plantar sensation of both feet was evaluated using Semmes-Weinstein Monofilaments (SWM) by applying them to the base of the heel with sufficient force to bend the filament. Participants were asked to indicate if they could feel the monofilament during three trials. Sham applications, where the monofilament did not touch the skin, were randomly included in the testing procedure. A correct response on two out of three trials was required to consider the sensation intact for a particular monofilament size. The procedure was repeated with monofilaments of varying thickness (based on initial performance) until the individual failed to detect the monofilament correctly on 2/3 trials. The minimal detectable change (MDC) of the evaluator size for SWM was 1.28-1.79 in the inter-rater test and 1.942.06 in the intra-rater test [14]. The marker value of the last correctly detected monofilament was recorded as the individual’s threshold for detecting cutaneous stimuli. Marker values were calculated using the equation: marker value = log10 [force (in mg) x 10]. Scores for this test range from 1.65 to 6.65 log(mg), with higher scores indicating reduced cutaneous sensation [15].
Gait Assessment and Intervention Tool
The Gait Assessment and Intervention Tool (GAIT) is employed to rigorously evaluate gait function using a 31-item scale, which is segmented into three distinct parts: assessment of the upper limb and trunk, the lower limb during the stance phase, and the lower limb during the swing phase. Each item on the GAIT is rated on a scale from 0 (indicating normal gait) to 3 (indicating maximum deviation), providing a detailed measure of gait abnormalities [16]. For precise gait analysis, two video cameras set at a frame rate of 60 Hz with MPEG-2 standard definition output were used. The cameras were strategically positioned to capture comprehensive gait movements from both sagittal and frontal planes. The first camera was placed 1.5 m from the centre of the walkway to record lateral movements as participants passed by, while the second camera was positioned 8.5 m from the centre, capturing frontal movements as participants walked directly towards it. Both cameras were mounted on stable tripods, each with a height of 80.5 cm from the floor [17]. The captured video data were analysed using Kinovea® software (version 0.8.15, available at http://www.kinovea.org), which allows for detailed examination and measurement of various gait parameters, facilitating an accurate assessment of gait dynamics and deviations.
10-Metre Walk Test
The 10-Metre Walk Test (10MWT), a commonly used method for assessing walking speed, was employed in this study. Participants were instructed to walk 10 m unassisted, with the time measured for the intermediate six metres to account for acceleration and deceleration. Assistive devices were permitted if needed, though the same device had to be used consistently and noted in the documentation for each test. Timing commenced when the participant’s toes crossed the two-metre mark and concluded as the toes passed the eight-metre mark [18]. Each participant completed three trials at either their preferred or maximum walking speed, which was documented. The average time from the three trials was then calculated to determine their typical walking speed.
Timed Up and Go
To assess the Timed Up and Go (TUG) test, a chair was positioned against a wall, and a line was drawn three metres away from the chair. Participants were instructed to sit in the chair with their arms resting on the armrests and their backs straight. On the command “go” from the researcher, participants stood up, walked to the line, turned around, walked back to the chair, and sat down as quickly and safely as possible. A stopwatch was used to record the time taken for each trial [19]. The TUG test evaluated mobility and balance by measuring the time it took to complete the sequence of actions. Each participant performed three trials, and the average time was calculated and recorded.
Data analysis
The data were analysed using GraphPad Prism version 9.5.1 (GraphPad Software, CA, USA). Participant demographics and clinical characteristics were summarised using mean and standard deviation (SD) or frequency and percentage (%), as appropriate. The Shapiro-Wilk test assessed the normality of data distribution. Changes from baseline were calculated for all outcomes at four weeks and eight weeks. Subsequently, a two-way mixed analysis of variance (ANOVA) was performed, followed by Fisher’s least significant difference (LSD) test for multiple comparisons to evaluate the outcomes. The study adhered to the intention- to-treat principle; analyses included all participants as originally assigned, using the last observation carried forward method to handle dropouts. This approach maintains the integrity of the randomised allocation and the validity of the study results. Statistical significance was established at a p-value of less than 0.05.
Results
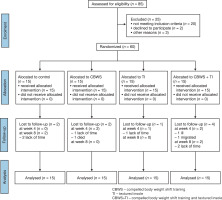
As indicated in Figure 2, 85 individuals were assessed for eligibility to participate in the study. of these, 25 were excluded, with 20 not meeting the inclusion criteria, two declining to participate, and three excluded for other reasons. Consequently, 60 participants satisfied the inclusion criteria, were enrolled, and randomised into four groups (control, CBWS, TI, and combined; n = 15 each). All participants received their allocated intervention, though nine dropped out during the study (two in the control, two in CBWS, one in TI, and four in combined). The reasons for dropout varied, including lack of time, illness, migration, and death. The analysis was conducted using the intention-to-treat principle, with the last observation carried forward to account for participants who dropped out. This method ensures that all participants initially randomised were included in the analysis, preserving the benefits of randomisation and maintaining the integrity of the study results.
Baseline participant characteristics were analysed, and there was no significant difference observed between the groups, except for the paretic side (Table 1), indicating that the groups were generally comparable at the start of the study. Throughout the study, there were no reports of serious adverse events, indicating that the interventions were well-tolerated by the participants.
Table 1
Participant characteristics
For the FMA-LE, there was an increase in the score starting at week eight after intervention in the control, TI, and combined groups. Additionally, the score at weekeight showed an increase compared to week four in these three groups (Table 2). There was a significant difference between control vs combined (p = 0.021, ES = 0.67), CBWS vs combined (p = 0.009, ES = 0.77), and TI vs combined (p = 0.027, ES = 0.62), with the combined group showing the highest scores at week eight (Figure 3A). The results indicate that the combined intervention of CBWS and TI had a superior effect on improving lower extremity motor function than the other interventions.
Figure 3
Comparative effects of different interventions over eight weeks on lower limb motor and sensory function. Panels depict changes in (A) Fugl-Meyer Assessment - Lower Extremity (FMA-LE) and (B) Semmes-Weinstein Monofilaments (SWM) across the control (control, purple), compelled body weight shift training (CBWS, blue), textured insole (TI, green) and compelled body weight shift training and textured insole (CBWS+TI, orange) groups

Table 2
The mean of change of all outcomes in different interventions over eight weeks
For the SWM, there was only an improvement in the combined group at weeks four and eight compared to the baseline (Table 2). At eight weeks, there were significant differences between control vs combined (p = 0.020, ES = 0.62), CBWS vs combined (p = 0.015, ES = 0.72), and TI vs combined (p = 0.004, ES = 0.61) (Figure 3B). These findings suggests that the combined intervention was particularly effective in enhancing somatosensory function.
For the GAIT score, there was a significant reduction starting at week four, becoming more pronounced at week eight after intervention in all four groups (Table 2). Additionally, the score at week eight showed a significant reduction compared to week four in all groups. However, no significant difference was observed between the groups (Figure 4A). These results suggest that all interventions, including the control condition, were effective in reducing gait abnormalities over time.
Figure 4
Comparative effects f different interventions over eight weeks on gait quality, gait speed, and functional mobility. Panels depict changes in (A) Gait Assessment and Intervention Tool (GAIT), (B) 10-metre Walk Test, and (C) Timed Up and Go test (TUG) across the control (control, purple), compelled body weight shift training (CBWS, blue), textured insole (TI, green) and compelled body weight shift training and textured insole (CBWS+TI, orange) groups

For the 10MWT, there was an increase in gait speed at week eight after intervention compared to baseline in the control and CBWS groups (Table 2). There was a significant difference between control vs TI (p = 0.022, ES = 0.73) and control vs combined (p = 0.037, ES = 0.60). However, no difference was observed in the TI or combined groups (Figure 4B). These results suggest that, while CBWS alone was effective in improving gait speed, the combined intervention did not show additional benefits over the control condition.
For the TUG test, there was a significant reduction in the time to perform the TUG at weeks four and eight after intervention, compared to the baseline in the control and CBWS groups (Table 2). There was a significant difference between CBWS and TI at week eight (p = 0.028, ES = 0.56). However, no difference was observed in the TI group or in the combined intervention group (Figure 4C). These results show that CBWS alone was effective in improving functional mobility, whereas the TI and combined interventions did not provide additional benefits.
Discussion
The present study assessed a new technique that integrates plantar somatosensory stimulation with CBWS. Specifically, this combined treatment was intended to evaluate lower limb motor function, gait, and sensation of stroke patients over eight weeks. The study results showed that the combined group achieved better outcomes on the FMA-LE and SWM scores than other groups, portraying better motor and sensor functions. However, additional training did not result in an increase in gait speed and functional mobility when compared to either individual treatments or none. This emphasises the importance of using sensory stimulation techniques with CBWS for better motor and sensor functions during stroke rehabilitation.
At eight weeks, there were significant improvements in the FMA-LE scores of the control, TI, and combined groups. However, the highest percentage change was observed in the combined group. Moreover, FMA-LE scores were significantly different between the control and combined, CBWS and combined, and TI and combined groups, reflecting that the combined intervention of CBWS and TI had superior effects on lower extremity motor function than any other interventions. This might be attributed to the synergistic effect of enhanced sensory input and weight distribution, leading to improved motor control and coordination. Indeed, Wang et al. [20] also noted improved FMA-LE scores in stroke patients with customised insoles. Indeed, this enhanced somatosensory feedback from the plantar stimulation combined with forced weight shift might have afforded more effective motor relearning. These findings confirm previous reports of multi-modal interventions, including sensory stimulation combined with task-oriented training that enhanced neuroplasticity and functional connectivity in the brain to promote motor recovery [21].
Only the combined group showed significant improvement in SWM scores, which was during weeks four and eight. At eight weeks, differences were found between the control and combined, CBWS and combined, and TI and combined. Therefore, the combined CBWS and TI intervention effectively enhanced somatosensory function. Such an improvement in somatosensory function can be relevant for balance and gait since this kind of sensory input from the feet plays a crucial role in postural stability and coordination of movement. Without a clinically significant change in the TI group in isolation, it might mean that TIs cause increased sensory input, which may not be sufficient for clinically meaningful changes in sensory function without the inclusion of CBWS. This adds to the results of an earlier study indicating that a high-intensity multidisciplinary rehabilitation programme significantly improved motor and gait outcomes in patients with functional movement disorders [22]. The CBWS component most likely facilitates the effectiveness of sensory interventions, as the latter increases better weight distribution and stability, which can facilitate the integration of sensory feedback into functional movements.
The GAIT scores improved in all groups at four and eight weeks, with statistically significant changes from baseline, but did not differ significantly between the groups. This indicates that the interventions enhanced gait over time, but no single intervention approach was superior. These findings are contrary to those by Aru- in and Kanekar [23], who recorded an immediate effect of TIs on the symmetry of gait in healthy persons. Perhaps the lack of differences in our study comes from the chronic condition of participants, and longer or more intense interventions might be required. Improvement in the control group further indicates that general physical activities, complemented by a structured walking program of 2,000 steps three times a week, accounted for general gait improvement, highlighting the importance of regular exercise in stroke rehabilitation.
The gait speed was significantly higher at week eight compared with baseline on the 10MWT in both the control and CBWS groups and showed significant differences between the control and TI and control and combined groups, but not between the TI and combined groups. While CBWS alone improved gait speed significantly, the combined intervention (CBWS+TI) did not demonstrate significant superiority compared to individual interventions, suggesting a potential complexity in integrating sensory and motor interventions. The observed limited superiority of CBWS and TI contrasts with Kim and Jang [24], who reported improvements in task-oriented and cognitive sensorimotor training. This discrepancy may reflect the need for tailored integration of sensory and motor interventions to maximise their synergistic effects. In a similar study, Aruin and Rao [25] reported notable improvements in gait velocity four months after the intervention when using TIs for six weeks of treatment. Conversely, our results align with Mohapatra et al. (2012), who reported significant increases in gait velocity in acute stroke patients after a two-week intervention with CBWS [11]. A similar course of six-week CBWS physical therapy in chronic stroke patients also showed continued gains in gait velocity at three months follow-up [10].
The reasons for the lack of further gains in gait speed from the TI and combined CBWS and TI interventions might be due to complexities in integrating both approaches, which served to dilute their individual benefits. While CBWS enhanced weight distribution and stability, and TI increased sensory feedback, the combined intervention may have needed more time for adaptation or a different protocol for their full synergistic effect to become evident. Future research is necessary to test multiple combinations and intervention durations of CBWS and TI to identify the optimal combination for improving gait speed post-stroke. Moreover, an investigation of the mechanisms through which such treatments alter the dynamics of gait could provide valuable insights into which one may further optimise rehabilitation strategies.
In the TUG test, which reflects mobility, balance, and fall risk, the CBWS intervention significantly improved dynamic balance and mobility, an essential factor for daily activities and reducing fall risk in stroke patients. The moderate improvement in the TI and combined groups suggested that sensory interventions alone or in combination with CBWS do not enhance functional mobility as much as CBWS does. This may be because the TUG test depends more on motor control and stability rather than sensory feedback. Similarly, Aruin and Rao [25] found that TIs made no difference in the performance of TUG in stroke patients. The limited gains observed with CBWS and TI may be due to complexities in integrating sensory and motor interventions, potentially diluting their individual benefits. Future studies should explore variations in intervention protocols, such as longer durations or sequential approaches, to identify strategies that optimise functional outcomes. Moreover, it may be worth investigating other dimensions of functional mobility, such as endurance and muscle strength, for an in-depth insight into how these interventions affect general mobility and independence in stroke patients.
The study was the first to evaluate the combined effects of CBWS and TI on lower limb motor function and gait in stroke patients. The randomised controlled design and multiple outcome measures strengthen the validity of the findings. However, several limitations must be acknowledged. First, the study did not include a follow-up period to determine whether the effects of the intervention persisted over the long term. Future research should incorporate follow-up assessments to evaluate the sustainability of improvements and investigate whether these translate into functional gains, such as reduced fall risk and improved independence in daily activities. Second, the dropout rates and reasons varied across groups, with the combined group experiencing higher attrition due to factors such as lack of time, illness, and migration. While some of these factors are uncontrollable and unrelated to the intervention, they may still influence the study’s statistical power and generalisability. Regardless, intention-to- treat analysis was applied to mitigate these effects. Future studies should consider strategies to minimise dropout rates where feasible and evaluate how intervention-specific demands impact adherence.
This study was conducted in Nigeria, which may limit the generalisability of the findings to other healthcare systems or populations. The sample size was calculated with an assumed 20% attrition rate, ensuring adequate power to detect statistically significant differences. Importantly, the actual dropout rate was lower than expected at 15%, indicating that the study maintained sufficient statistical power despite the uneven distribution of dropouts across groups. However, the relatively small number of participants per group (15 per group) remains a limitation. Future studies should incorporate larger sample sizes and be conducted across multiple and diverse settings to enhance external validity. Additionally, future studies should explore the mechanisms underlying the observed improvements in sensory function, as these insights could inform the development of more effective rehabilitation strategies.
Lastly, further research should examine various combinations and durations of interventions to optimise rehabilitation outcomes for stroke patients.
Conclusions
Plantar somatosensory stimulation combined with CBWS and TI was associated with a relatively significant improvement of lower extremity motor function and somatosensory function in stroke patients. The combined group demonstrated significant improvements in motor function (FMA-LE scores) and sensory function (SWM scores), highlighting the combined intervention’s effectiveness in addressing both domains. However, the combined intervention did not improve gait speed or functional mobility (as assessed by the 10MWT and TUG tests) beyond the benefits of individual interventions or the control condition. This evidence points to combined CBWS and plantar somatosensory stimulation as a potential rehabilitation strategy in the improvement of motor function and gait in stroke patients.