Introduction
Sports injuries are injuries that occur during the practice of physical exercise or sports activities. Head injuries can occur due to a lack of training while practicing or the unavailability of the desired equipment [1]. Adults are less likely to experience sports injuries than children, whose susceptibility is intensified by immature reflexes, an inability to detect and measure risks, and underdeveloped coordination [2]. Injury rates are higher in contact sports, and the most severe occur in individual sports modalities.
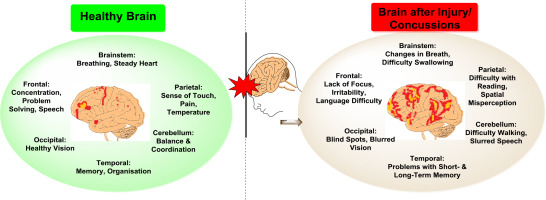
In recent times, special attention has been paid to sport-related brain injuries. Moreover, ligament injuries (i.e., sprains), bone injuries (i.e., stress fractures), and muscle injuries (i.e., strains) are also highly prevalent sports injuries. One of the main acquired brain ailments with debilitating effects on all population segments is traumatic brain injury (TBI). Healthcare professionals have also identified TBI as a significant cause of death and disease/illness in young adults [3–8]. TBI has also been reported to contribute to the early onset of brain disorders such as dementia and Alzheimer’s [9, 10]. Another major concern is concussions in sports. According to the Berlin consensus statement on concussion in sports, a concussion is a TBI induced by biomechanical forces [11]. A direct hit to the head or body may cause a concussion. A concussion is caused by direct or indirect external trauma to the head, resulting in shear stress to brain tissue from rotational or angular forces. The symptoms often include fatigue, drowsiness, ringing in the ears, nausea, headache, blurry vision, and vomiting [12]. Figure 1 depicts a comparison between a healthy and an injured brain.
TBI is a major cause of death and disability and a significant health and socioeconomic problem for our society. Brain injuries are becoming increasingly common in athletes and represent an important diagnostic challenge. Early detection and management of brain injuries in sports are of utmost importance in preventing chronic neurological and psychiatric decline [13]. In this overview, we have attempted to describe sports-related head injuries, including traumatic injuries of the head. This review aimed to provide insight into the types and frequency of brain injuries. The article covers brain-related injuries associated with the 16 sports with the highest injury incidence. Those aspects are discussed in detail. Each sports discipline is treated individually with some case studies. The sports included in the present study are sorted alphabetically for easy reading and understanding. A subpart mentioning the management of brain-related sports injuries, including pharmacological management, was also included in the manuscript.
Head injuries in sports
Baseball
Baseball is a non-contact sport. Even so, frequent concussions and other head injuries have been reported in baseball players. Over six million children participate in professional baseball leagues each year, and up to thirteen million more play non-organised games. The upper and lower extremities are the most affected area while playing sports, such as baseball [14]. Traumatic brain injuries are the most common type of injuries in baseball. Almost 110,000 children aged 5 to 14 were treated in 2009 for baseball-related injuries in hospital emergency rooms. It also has the highest fatality rate among sports, with three to four children dying yearly from baseball injuries [15, 16].
Many studies published over the last ten years have listed 242,731 TBIs associated with baseball and soft-ball [12]. In young players, the leading cause of head injuries is striking the bat on the head. Injury incidence rates are higher in matches than in practices. The number of injuries occurring in women is almost twice as high as in men while playing baseball. Different degrees of severity can occur, ranging from minor to severe. Therefore, multifaceted preventive strategies must be implemented to reduce the frequency and burden of these injuries [17]. In a recent survey, it was verified that baseball has the third highest incidence rate (after cycling and soccer) among all sports injuries requiring hospital emergency care or medical evaluation [18].
Basketball
Basketball is a highly competitive sport where physical pressures are continually associated with the knee joint [17]. Traumatic injuries associated with basketball result from specific technical movements [19]. Compared to other sports, such as football or wrestling, the incidence of head trauma in basketball players is less common, while muscular injuries in different body parts are very frequent while playing basketball [20, 21].
A European survey report ascertained that 1.6 million involved in basketball are examined at emergency departments every year. Head and neck injuries present the highest incidence rate, particularly in youth players, and quite frequently, those individuals require treatment or evaluation by emergency medical services [22]. It has been reported that the number of concussion incidences among National Basketball Association (NBA) players was approximately 17 instances per season (among 149 players) since 2011, caused by biomechanical forces [23].
One of the studies revealed that 10–20 years old individuals are more prone to head injuries from basket- ball. Another study reported that collegiate females have more concussions (9%) when playing basketball compared to males (5%) [24, 25]. Moreover, it was also found that the average number of games missed after a concussion by NBA players was 1.6 from 2006 to 2014 [26–28].
Boxing
Boxing is a full-contact combat sport in which two players wearing gloves punch each other in a ring for a predetermined time. Most of the casualties in boxing suffer from traumatic brain injuries. Clinical data showed that boxers suffer repeated concussions, some of which last long periods [29].
When a boxer has a series of concussions, the corpus callosum (CC) develops micro-structural neuropathology and can become dose-dependent, according to Ware et al. Diffusion Tensor Machines (DTM) are used to examine e-boxers. The results showed that repetitive head injuries cause many effects on splenium and, to some extent, cause chronic injuries. In addition, executive dysfunction and depression cause high CC disruption [30].
The Armed Forces Health Surveillance Center (AFHSC) reported that practicing combat sports creates higher risks of sports-related injuries among military members. High indices of injury are commonly reported in combat sports. Sprains, strains, and contusions were diagnosed, which were associated with combat sports. It was also verified that the most severe injuries, such as concussions, skull or face fractures, and intracranial injuries, occur in boxers [31].
Cheerleading
Cheerleading has developed into a complex sport utilising aspects of gymnastics/tumbling, dance, single- and multiple-partner stunts, and tosses in complex displays [32].
Cheerleading has become much more than shouting encouraging phrases from the sidelines. However, safety is also essential for cheerleaders, even with overall rates of injuries lower than in other high school sports [33].
The overall injury rate in cheerleading is 0.71 per 1000 athlete-exposures (AEs). Although the number of injuries among cheerleaders is low, whenever they do occur, they are severe [34–36].
The American Association of Neurological Surgeons reported that cheerleading is among the top 20 sports with a maximum head injury rate. Studies show that cheerleaders have the highest risk of concussions (14 per 100,000) [37].
The factors responsible for the higher risk of injuries in cheerleading include BMI, previous injuries, stunt performance, cheering on hard surfaces, and not having a higher level of training and experience, either under coach supervision or by themselves. A concussion is the most common injury reported in cheerleading. One recent study reported that male cheerleaders are injured more frequently than female cheerleaders [38].
Other severe injuries that cheerleaders confront include fractures resulting in paralysis and spinal cord contusions with transitory or resolving symptoms [39].
Cricket
Cricket has become a global sport, and millions of people from 104 countries are affiliated with the International Cricket Council (ICC) [40]. Since cricket is a non-contact sport, overuse and impact injuries become very common because players engage in many other physical activities, including throwing, catching, running, batting, bowling, diving, and jumping. Technique, physical fitness, and strategy are the foremost requirements for cricket [41].
From 1870 to 2015, professional international cricket reported 36 catastrophic head injuries; five were fatal, accounting for 14% of the total injuries, and nine were career-ending, accounting for 22% of the total injuries [42]. An incident was reported where a 24-year-old male athlete was injured by a cricket bat while training and was hospitalised with an open head bleeding trauma in the middle part of his right eye [43].
It was reported that males experience more injuries than females (3583 male injuries vs. 324 female injuries). The rate of injuries was 1.3 and 0.4 per 1000 participants for males and females, respectively [44]. It was observed that when the players were batting, most of the injuries occurred in the head and neck. No injuries have been reported by umpires [45–47].
In recent times, cricket has given rise to concern since many high-level players are getting injured [48–50].
In a Premier League match, one South African cricketer lost his life after being hit on the head while batting. The 32-year-old player was severely hit on the side of his head. He collapsed immediately, and although he was sent immediately to the hospital, the medical staff failed to revive him [51]. In another incident, an Australian batsman died from a head injury [52].
Diving
Diving involves immersing oneself underwater, whether in rivers, lakes, or seas, with the aid of underwater breathing equipment, to explore underwater landscapes. The most common diving-related injuries are loss of hearing and vertigo. Proper diagnosis and accurate treatment help scuba divers prevent long-term diseases and impairments [53].
A detailed study of scuba diving injuries in the Canary Islands was reported. This study revealed that 71% of injuries occurred in men. 43% of the divers had type 1 decompression sickness, and 52% comprised type 2, while the rest showed omitted decompression [54–60]. Cilveti et al. discussed the physiology and risks of scuba diving in children and listed some recommendations for children while practicing with compressed air. Underwater physiology is an essential factor to be entirely understood before diving. The information on the environmental forces that act on the divers helps prevent injuries [54–60].
A concussion study was performed on 24 divers, and the data showed that 54.2% of the participants had had a diving-related concussion. The three most common symptoms reported were headache, dizziness, and difficulty concentrating, all occurring in 91.7% of the concussions. On average, it took 23 days for the divers to return to practice. Most divers reported being unconfident about performing the dive, which resulted in a repeat concussion [61].
American football
American Football is a highly dynamic sport, having significant physical contact and greater risks of brain injuries. A large number of traumatic brain injuries are caused by football. In the case of American-style football, there is a considerable risk of Repetitive Head Impact (RHI) exposure, which results in acute and chronic brain injuries [62].
In a US report, 1.6 to 3.8 million concussions occur yearly in sports and recreational activities; further, SRCs (sports-related concussions) affected more than 5% of college and high school football players [31, 63].
It was observed that repeated concussions, related to repetitive head injuries that happened to a 25-year-old man while he was playing American football, might have resulted in learning and behavioural issues, as confirmed in an autopsy. He had a neurodegenerative disorder and chronic encephalopathy [64].
Football players suffer subconcussive impacts throughout the season, which increases serum neurofilament light (NfL), a biomarker for axonal injury [65].
A survey mentioned by the Journal of the American Association analysed the brains of 202 injured people who played football at various levels [66]. The data indicated that there were 0.41 concussions per NFL game in American football: Impacts caused by other players’ helms represented about 67.7% of the concussions. About 2.4% having concussions were taken to hospital, and 9.3% involved unconsciousness. It was observed that around 92% of those who sustain concussions return to practice within seven days [67, 68]. A study observed that, on average, a head injury occurs in every third match during international football tournaments [69].
NFL data reported that players who got concussions while practicing decreased in 2018, as there were 281 total cases, and there were 214 in 2017, which then further increased to 224 in 2019 [70]. Concussions are the most common injury in American Football, and around 200 NFL players suffer yearly [71]. Athletes aged 18 have higher risks for concussions. This rate is double that of 13-year-old players. In addition, girls face a 1.5 times greater risk of concussions than boys.
The maximum injury rate and the highest severe injury rate found among American Football players were 3.87 per 1000 athlete-exposures [AEs] and 0.80 per 1000 AEs, respectively [72]. Moreover, it has been reported that younger players (under eight years of age) suffer more head injuries than other age groups, based on a retrospective review of the charts, and football injury rates in adolescents and children are not significantly conditioned by age [73].
Golf
Golf is a game of club-and-ball where players hit the ball into various holes in mini-mum strokes by using various clubs. Head injuries are reported in golf, and involve golf club, golf cart, and golf ball trauma [74]. Children have higher risks of suffering TBI caused, particularly to the head and neck, by golf carts [75]. A study reported that about 70% of children sustained TBI from a fall [76]. Another study analysed golf-related injuries treated in US hospital emergency departments using the National Electronic Injury Surveillance System database. The study indicated that 18–54 years old patients accounted for 42.2% of injuries. However, injury rates per 10,000 golf participants were higher among individuals aged 7–17 (22.1) and ≥ 55 years old (21.8), compared with subjects aged 18–54. Injured by a golf club (23.4%) or struck by a golf ball (16.0%) were the most commonly specified mechanisms of injury. The head/neck was the most frequently injured body area (36.2%), and sprain/strain (30.6%) was the most common type of injury. Most patients were treated and released (93.7%), whereas 5.9% required hospitalisation [77–79].
Gymnastics
Gymnastics is also a high-risk sport for head and neck injuries [80]. A study from 2001 to 2011 reported that 64 males and 55 females sustained 240 and 201 injuries, respectively. The injury rate observed was 8.78 per 1000 AEs for males and 9.37 per 1000 AEs for females [81]. Female gymnasts suffered more injuries than males and underwent major surgeries, with rates of 24.4% for females and 9.2% for males [82]. In gymnastics, common injuries include muscle soreness, contusions, back injuries, over-training syndrome, ankle sprains, wrist sprains, head, neck, and shoulder injuries [83].
Hockey
Hockey is a team sport where the players try to shoot the ball or puck into the opponent’s goal with a hockey stick. The types of hockey include bandy, ice hockey, field hockey, and rink hockey.
Furlong et al. [84] investigated the types of injuries and injury ratios in males and females. They also estimated the number and types of injuries in youth field hockey in major international championships. It was observed that girls were more prone to minor injuries than boys. Most injuries, including contusions, were caused by ball or stick impacts. The injury ratio observed for boys was 53 injuries per 1000 players during games and 86 per 1000 for girls. The highest number of injuries occurred in the trunk, which includes the thoracic and abdominal segments [84].
Athletes participating in contact sports such as ice hockey have greater risks of concussions. Donaldson et al. [85] studied concussion cases in two major leagues, NHL (National Hockey League) and OHL (Ontario Hockey League). Differential data were compared, and it was observed that 64.2% of NHL contusions were caused by body checking, and 28.4% of contusions and 36.8% of suspected concussions were caused by illegal incidents [85].
The reliable change indices (RCIs) were calculated and showed that acute loss of consciousness, amnesia, or any postural instability can result in severe injury and require intensive cognitive follow-up [86]. When Brunner et al. [87] investigated the epidemiology of traumatic injuries and overuse injuries in some Swiss ice hockey players. They observed that concussions and muscular strains were the most time-consuming ailments, with the hip and groin regions being the most impacted.
According to the research, most of the injuries in Inline Skater Hockey were minor bruises, abrasions, and cuts. Differential data was collected on various injuries that were comparable to ice hockey. Moreover, following all protective measures, the risks of suffering head injuries can be significantly reduced [88]. Rink Hockey Players who use a hard ball and wear little or no protective gear have high rates of concussions and head injuries. A cross-sectional epidemiological study indicated that head injuries were the most frequent type (20.8% of all injuries). Concussions comprised 7% of all head injuries with a rate of 0.76/1000 per athlete exposure. Ball contact was the cause of 31% of injuries, while player contact generated 26.2% of all injuries. There was not much difference observed in male or female injuries. In this high-speed and low-contact sport, the majority of injuries were due to contact with the ball [89].
In a case study, the frequency and impact of head injuries were studied by Chen et al. between Pee Wee players and Bantam ice hockey players. The investigation results showed that Pee Wee players suffered severe impacts on their heads from elbows and boards.
By contrast, bantam players experienced strong impacts on the glass [90].
A test method was developed by Post et al. [91] for evaluating helmet standards in ice hockey. To calculate the brain tissue strain, linear acceleration and rotational acceleration time curves were used. The newly designed test protocols effectively displayed the levels associated with concussion in ice hockey [91]. It was observed that the rate of injuries was higher in competitions compared to practices. In addition, there were many concussions cases for which various strategies were required to prevent injuries [92].
Among junior hockey players, a quantitative electroencephalograph (qEEG) was utilised to determine the severity and chances of concussions. The most injured sites observed were F8, T6, O1, O2, and F7; that is, the right side of the head, the back of the head, and the left front of the head [93]. Furthermore, on analysing some of the junior ice hockey championships, it was observed that junior male players have a lower risk of injuries than adult males but have a higher risk than women [94].
Karate
Karate is a martial art and self-defence system very popular internationally. Karate means ‘empty hands’, which is fighting with an opponent without using weapons [95]. In Karate, on average, there is one injury for every eleven bouts. That is, one for every twenty-five minutes of effective fighting with an opponent. According to the severity level, all were minor or mild [96]. Participation in this sport has significantly increased over the last 10–15 years, with approximately 8 million American participants in more than one style.
The injury risk is twice as high in the age group of 12–17 years than in the 6–12-year-old group. Girls also present a higher injury risk than boys. Similarly, youngsters and female athletes are likely to suffer more head injuries than males and children [97, 98]. Some case reports involving head injuries with Judo Karate are shown in Table 1.
Table 1
Head injuries in karate: case report
| Researcher, year | Area | Player | Practice/play | Injury |
|---|---|---|---|---|
| Galvez, 2011 [98] | USA | 41/male | karate training | Haematoma (haemorrhage intracranial) (subacute subdural) kick to kick pad at high speed |
| Moran, 2013 [99] | USA | 50/male | karate training | Kick to head leading to superficial temporal artery traumatic AV fistula |
| Nandi, 2016 [100] | India | 10/female | pactice, pain in neck, restricted movement of neck after punch | ‘Backward bending’ in MRI of odontoid process, kinking of medulla oblongata |
McPherson et al. [101] reported that injury rates in males and females were, respectively, 2300 and 1033 per 10,000 (0.3% participation), and 575 and 258 per 10,000 (1.2% participation). Injuries are more frequently reported in karate compared to other sports (33%). The most common mechanisms of injury were falls, throws, and jumps (33%). Fractures (20%) were the most frequently reported type of injury, and the lower limb was the most frequently injured area of the body (41%) [101, 102].
Mountain climbing
Mountain climbing, often known as mountaineering, is a pastime in which a person enjoys ascending to higher mountain elevations [103].
Every year, several injuries associated with rock climbing result in visits to US Emergency Departments, with an average (SD) ranging from 3023 (149) to 3816 (854). Schussman et al. observed an incidence of around 2.5 for every 1000 mountain climbers and 5.6 for every 10,000 hours [104]. According to Lack et al. [105], there is a higher probability of suffering injuries around 3:00 pm during the summer, autumn, and spring. Concussions and facial lacerations are the most common causes of head and neck injuries. Males present a higher prevalence than females and also suffer more severe injuries [106]. These injuries primarily affect young men, although the injuries sustained are not particularly serious [107].
Rugby
Rugby is a close-contact sport where the objective is to ground the ball behind the opponent’s try line. In rugby, concussions are a big problem among elite players [108, 109]. Rugby is becoming increasingly popular among athletes, from high schools to colleges. The head and neck are the most injured body areas in rugby, with tackling being the most common cause of injury [110–113]. Injuries among men are 30% more frequent than in women [114].
Head injuries range from trivial face injuries, scalp lacerations, and broken noses to serious concussions [114]. This is a common side effect of rugby, resulting in injuries to the face, scalp, nose, and concussions. According to certain studies, rugby accounts for 20% of all sports injuries. According to research, one out of every four players sustains an injury when performing 20–40 tackles each match in one season [115, 116].
Females are more likely than males to have head and neck injuries, with a rate of 16% compared to 5% for males [117].
Almost 15–30% of the injuries are quite severe, and if the player returns very quickly after an accident, there is a higher risk of suffering a similar injury [118].
Soccer
Soccer is the fastest-developing and most popular sport nowadays [119]. Soccer may lead to head injuries caused mainly by ball-head impacts or repeated intentional head impacts while heading the ball [120]. The American Academy of Pediatrics in the USA has ranked it at the same level as ice hockey and American football in terms of incidences reported [121, 122]. Head and neck injuries are the most common in soccer, ranging from 4 to 22%, which represents an incidence of 1.7 injuries per 1000 in games and 0.5 per 1000 in practices [123, 124]. Consumer Product Safety Commission (CPSC) statistics state that 40% of the concussions occur when the player’s head impacts another player, whereas head to the ground represents 10.3% of the total injuries [125]. Men suffer more concussions than women (10.2 in 10,000 games versus 8.4 in 10,000 games) [126]. A recent study from Victoria, Australia, revealed that head injuries are more common at the age of 10–14 than at the age of 5–6 [127].
Volleyball
Volleyball is not a contact/collision sport. Even so, injuries with different degrees of severity occur. These injuries include those to the nerve of the brachial plexus and concussions, representing 4% of the total injuries in collegiate-level female volleyball players [128]. Ball-to-head contact is the most common mechanism of injury, followed by player-to-player contact and player-to-floor contact [129]. The risk of injury is higher among centre players and lower for liberos [130]. Most ball-contact injuries were to the hand/wrist (32.7%) and head/face (27.0%) and were diagnosed as contusions (30.5%), sprains (23.1%), and concussions (16.1%). Women are more prone to suffer concussions than men, and the net range of injury, according to the NCAA, is 4.3 for every 1000 matches in women’s volleyball [131–133].
Wrestling
Wrestling has a history of head and neck injuries because it is a fairly physically demanding sport and requires strenuous training to improve strength, attitude, and psychological skills. Trauma in the CNS (central nervous system) that may lead to disability symptoms and severe injuries in wrestling affects 1 of every 100,000 players. Additionally, injuries are 80% more common in competition than during practice.
The injuries are not life-threatening in males and females and typically occur in the lower limb. In all wrestling disciplines, there is an increased probability of injury when the participant’s weight is lower than his or her opponent’s [134].
Head-to-head injuries occur mostly primarily at takedown, and severe injuries are secondary [135].
In a year, approximately 239,000 males and 1,700 females are wrestlers in high schools and 6,700 males in colleges [136]. During a competition, the probability of suffering a concussion is 6.6%, and 4.5% during practices [137]. The common concussion injury mechanism is a floor impact [138]. The mortality for all wrestlers over the 26-year study period was .007 deaths/ total person-years or 708 per 100,000 per year, and 16% of deaths occurred below age 50. Cumulative incidence function (CIF) and cardiovascular-related deaths in wrestlers are around 38% of the total number of deaths [139].
A summary of brain-related injuries in different sports, along with statistical data, is shown in Table 2. Table 3 summarises information about the differences between recreational and professional sports in each sport discipline and a comparison of brain injury occurrence by children and adults.
Table 2
Summary of brain-related injuries in different sports with statistical data
Table 3
Summary of brain-related injuries in different sports with statistical data
| Sport | Recreational vs. professional athletes | Children vs. adults |
|---|---|---|
| Baseball | High school females were at a higher risk of TBIs than males, with average injury rates of 0.10 and 0.04 per 1,000 AE, respectively [12] | |
| Basketball | Children and adolescents received head injuries more often compared with the other age and skill categories [18] | |
| Boxing | From 1932 to November 2007, 1465 boxing-related deaths were recorded worldwide. About 70% of these fatalities occurred in professional boxers. Although the number of fatalities has decreased considerably since 1960, it still averages about 77 deaths per decade [27] | |
| Cheerleading | Our findings concerning cheerleading injuries indicate that younger children (5 to 11 years old) are more likely to suffer moderate-to-severe injuries https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5805112/ | |
| Cricket | The incidence of concussion in cricket is not known [39] | In previous nationwide surveys, Stretch and Raffan found that head and face injuries account for 9%-25% of injuries to batsmen. Emergency data collection in Australia from 1989 to 1993 mentioned that 44.4% of all cricket-related presentations in children and 16.6% in adults were for head injury [40] |
| Diving | ||
| American football | A 39% decrease in football-related traumatic brain injuries among children and adolescents helped cut the number of US emergency department (ED) visits for sports- and recreation-related (SRR) traumatic brain injury by one-third between 2012 and 2018 [66] The rate of closed head injury, which included concussions, was highest in the younger than 8-years-old age group [71] | |
| Golf | Patients 18-54 years old accounted for 42.2% of injuries, but injury rates per 10,000 golf participants were highest among individuals 7-17 years old (22.1) and 55 years old (21.8) compared with 18-54-year-olds (7.6) [77] | |
| Gymnastics | ||
| Hockey | Most injuries occurred to the head/face and shoulder/clavicle and resulted in concussions, contusions, or ligament sprains. Injury rates were higher in collegiate men than in high school boys during 2008-2009 through 20132014 (4.38 versus 2.33/1000 AEs; IRR = 1.88; 95% CI = 1.73, 2.05) [90]. The risk of injury among male junior ice hockey players was lower than the reported rates in adult men but higher than that in women [92] | |
| Karate | Those aged 18 had most of the injuries. The rate of injury was higher in athletes with weight less than 70 kg and lower sport experience (p < 0.05). The commonest locations for injury were the head and neck [93] The injury rate per exposure was generally higher for senior athletes than junior athletes (RRAE range: 1.03 to 1.75); however, when comparing injury rates accounting for exposure-time, the risk was generally lower for senior athletes than junior athletes (RRME range: 0.69 to 0.88) [94] The risk of injury for the 12-17-year-old age group was almost twice that of the 6-12-year-old age group, after accounting for exposure time (RRME 1.92 (95% CI 1.39 to 2.65)), and the difference was more pronounced for girls than boys (RRME 2.47 (95% CI 1.52 to 4.00) vs RRME 1.62 (95% CI 1.06 to 2.49), respectively) [95] | |
| Mountain Climbing | Technical roped climbers accounted for 58% of climbing victims, whereas unroped climbers accounted for 34% [103] | 46% of victims were between the ages of 20 and 29 years [103] Climbing accidents mainly affect young men [105] |
| Rugby | A higher level of play was associated with a greater incidence of injuries in matches, with no clear difference in severity [110] Professional-level injury rates were reportedly lower than semiprofessional participation [117] | |
| Soccer | Data suggests children are more susceptible to concussion from heading, primarily in game situations [119] The 10-14-years age group presented with more head injuries than the 5-9-years age group [125] | |
| Volleyball | ||
| Wrestling | ||
Overall remarks
No differences were found between contact and non-contact groups regarding treatment methods and recovery times [140].
Gender effects have not been as well studied as age and region of injury [22]. A suggestion has been made that females are at higher risk due to weaker musculo-skeletal support for the head, more perfusion cerebrally, and higher rates of glucose metabolism and circulating levels of estrogen and progesterone [22].
Injury rate is 2.7 higher during competition [141].
Management of brain injuries in sports
Non-pharmacologic strategies
Sports practice involves certain injury risks, with brain injuries being the most common at present. Hence, knowing the management strategies for sports-related brain injuries is essential. The most common brain injury in sports is a traumatic brain injury, which leads to disability and requires adequate management to alleviate symptoms since no treatment is currently available. Management of an athlete suffering a SRC includes looking out for signs and symptoms, including severe injury to the brain and spinal cord, and requires athletic rest. The history of brain injury must be considered since it might increase the severity of future brain injuries [142], their symptoms, and the mental and physical damage [143]. Observation for one month is essential if migraines or headaches occur at an early age [144]. One key aspect of managing concussions is assessing an individual’s condition and health history.
The Sideline 3 Concussion Assessment Tool and the NFL Sideline Concussion As-assessment Tool are commonly used to assess balance on multiple surfaces. The test consists of a balanced error-scoring system. Its duration is five minutes. It is performed in three standing positions, adopting single, double, and tandem stances [145, 146]. The Sideline Concussion Assessment Tool 3 is a new version of SCAT2, consisting of history related to health (i.e., migraine, attention, hyper-activity anxiety, or depression background). The most recent tool developed in 2016 is the SCAT-5. It has a different investigating process to assess cranial-level nerve function, consciousness, and other concussion-related symptoms. The new tool, Concussion Recognition Tool 5 (CRT5), has been updated from the Pocket Sports Concussion Assessment Tool, which can be used by the non-medical ‘lay-men’ staff [147, 148]. The management strategy should also consider not leaving the patient alone for one to two hours, and alcohol and other drugs must be avoided. The person’s activity should be increased gradually in 24 to 48 hours after cognitive and physical rest [149]. The more severe the case of brain trauma, the more complex the impairment of structure and function. This leads to a decrease in mental functioning [150]. Many emotional, behavioural, cognitive, language, and sensory functions can be affected, and pain is common in SRCs. Few athletes may require rehabilitation due to injuries in the cranial area after the trauma. Injured athletes may require extended periods to recover (from months to years) after a painful and severe case of TBI [151] or some complex medical condition [152, 153]. Doctors’ education related to brain injury and bio-psycho-social knowledge may help their patients recover faster and better during rehabilitation [154].
Brain injury management in sports includes different steps, such as checking the breathing pattern and cardiovascular system (CVS) function, testing the cervical spine, and reducing movement. If required, the patient must be transferred to the trauma centre. Also, decreased mental status and other possible neurological findings are taken into account. Diagnosis is not usually made by neuroimaging, which is used for some significant skull fractures in very severe brain injuries. Removal from sports competition in athletes presenting these injury symptoms is proposed by a healthcare professional with investigating experience in MTBIs [155]. In summary, concussion treatment is accomplished first with evaluation and diagnosis, then post-injury evaluation, and afterwards with symptoms management, and finally, a safe return to sports practice is proposed.
Pharmacological strategies
Some management strategies involve pharmacological parameters for the initial phase of brain injury management, focusing on individual symptoms. NSAIDs can be given if headache presents in the days after a concussion [156]. If the headache remains after that, then it requires treatment. Management comprises prophylactic medicines consisting of nonspecific β-blockers and tricyclic antidepressants. Persistent headaches after concussion should be managed as part of a comprehensive management plan for post-concussive syndrome [157]. When there is a concussion after a cranioencephalic trauma, there may be balance disorders that can cause vertigo. In these cases, meclizine and some benzodiazepines are the medicines frequently used.
The basic criteria for resuscitation are based on breathing, circulation, and airway. Cervical pain control with airway maintenance is necessary for patients with any head injury. Patients with a Glasgow Coma Score of no more than eight should be provided with assisted ventilation [158]. Anaesthetic drugs such as thiopental with suxamethonium can be used to combat a fatal increase in intracranial pressure [159]. Breathing and ventilation must be done to have a normal arterial carbon dioxide pressure of 4–4.5 kPa or 40 mm of Hg. Circulation is done by fluids and agents that alter the muscular contraction energy and should have 90 mm Hg (like the mean blood pressure of the artery) [160]. Oxygenated blood flow must be restored, preventing death from brain injury called secondary brain injury or neuronal death. In addition, cerebral perfusion pressure (CPP) must be maintained, as there is an almost 20% increase in mortality with each 10 mm Hg loss of CPP. Conversely, there is about a 35% reduction in mortality if the cerebral perfusion pressure is maintained above 70 mm Hg.
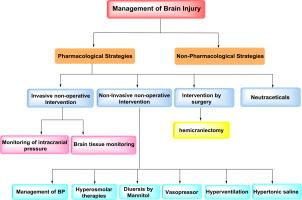
Invasive non-operative interventions
Intracranial pressure monitoring is necessary for non-operative invasive interventions while treating traumatic brain injury. There is a reduction in the mortality rate two weeks after injury if the intracranial pressure is monitored [161]. Clinical judgment of the Intra-Cranial Pressure (ICP) should be below 22 mm Hg. Above this level, there is an increased risk of death [162]. The best way of measuring the ICP is to insert a catheter into the third cerebral ventricle, called a ventriculostomy [163]. External ventricular drain (EVD), which is ventriculostomy, can also be used to treat intracranial hypertension. Using antimicrobial-impregnated EVD catheters may reduce the risk of ventriculitis. Jugular bulb oxygen saturation can also be monitored [164]. The Glasgow Outcome Score is worse when the venous saturation is lower than 50% at three months [165, 166]. This can be used to find out if the hyperventilation therapy is causing cerebral ischemia. Brain tissue monitoring and microdialysis catheters are newer options in invasive brain monitoring.
Non-invasive non-operative interventions
Management of BP and hyperosmolar therapies with the position of the head at 30 degrees, diuresis by mannitol, hyperventilation, and hypertonic saline can be overall used for the treatment of brain injuries [167]. It has become the standard for treating brain tissue movement, called herniation. Mannitol decreases the intracranial pressure in patients with TBI [168]. The endpoint of the TBI treatment is an osmolarity of 320 mOsm/L in serum [169]. Mannitol should not be administrated with hypovolemic shock during haemorrhages. Hypertonic saline increases the serum osmolarity without increasing or decreasing the intravascular volume. Hypertonic saline is prepared with 50% NaCl and 50% sodium acetate, decreasing the hyperchloremic acidosis [169, 170]. With the intake of IV fluids and vasoactive medicines, there is a rise in blood pressure. The drugs having the least effect on cerebral vasomotor are norepinephrine and phenylephrine, so these are preferred. With vasopressors, there is a need for simultaneous recording of haemodynamic monitoring with both a central venous catheter and a peripheral arterial pressure catheter [170]. Albumin increases the ICP more than saline, hence, it should be avoided while managing TBI [171]. Reducing the cerebral metabolic rate with anaesthetics and hypothermia anaesthetics, such as pentobarbital [172] or propofol [173], leads to a decrease in the rate of cerebral metabolic oxygen, ultimately reducing the cerebral blood flow, intracranial pressure and tissue oxygen demand. The high-dose barbiturates and propofol treat high refractory ICP compared with other therapies. However, there should not be any use of anaesthetics in prophylaxis against developing intracranial hypertension.
Interventions by surgery
When there is a high level of cerebral oedema, the best option is hemicraniectomy [174]. The chance of a positive outcome increases, and the mortality rate decreases. In stroke persons, decompressive hemicraniectomy has been beneficial. The continuous estimation of decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL), decompressive surgery for the treatment of malignant infarction of the middle cerebral artery (DESTINY), and hemicraniectomy after middle cerebral artery infarction with life-threatening edema trial (HAMLET) are recommended to show the benefits of a hemicraniectomy that is performed within 48 hours of acute ischemic stroke [175, 176]. For better results of hemicraniectomy, cranioplasty should be performed at the earliest opportunity, or it should be done with bone flap replacement [177, 178]. Intracranial pressure can also be treated with laparotomy as another potent option. A decrease in intra-abdominal pressure leads to a diminishing of the intrathoracic pressure, allowing a rise in venous drainage by cerebral veins, which can mainly result in a decreased volume of blood intracranially and so less intracranial pressure [179]. The management of brain injuries is depicted in Figure 2.
Nutraceutical
Nutraceutical research provides molecules from natural products that can be beneficial for brain function at the molecular level. Some naturally occurring molecules can be beneficial to both the young and aged brain, and these molecules aid in improving cognition or in managing debilitating neuropsychiatric and neurodegenerative conditions [180]. Dietary creatinine intake can raise brain creatine and preserve the brain’s cognitive function under stress. Consumption of creatinine is assessed in several adult neuro-degenerative conditions since it directly preserves mitochondrial function [181].
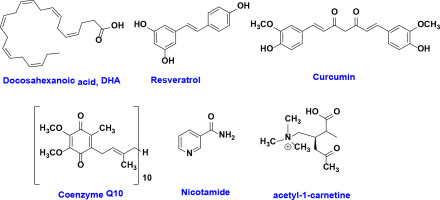
Other compounds, such as Omega-3 fatty acids (i.e., docosahexaenoic acid; DHA), control signal transduction and gene expression and protect neurons from death. In a recent study, it was examined that the capacity of dietary omega-3 fatty acids supplementation helps the brain cope with the effects of traumatic injury. Supplementation with Omega-3 fatty acids can restore cognitive function after TBI. Results also show that this diet can provide protection against oxidative damage after TBI, which may also influence synaptic plasticity and cognition [182].
Docosahexaenoic acid (DHA) is unique and plays multi-functional roles in sustaining brain health throughout the life span. DHA undergoes enzymatic and non-enzymatic conversions, forming oxylipins, which are powerful lipid mediators. An aldehyde derivative of DHA, 4-Hydroxyhexanal (4-HHE), can form adducts with DNA, proteins, and lipids. Oxidative metabolites of DHA regulate cell redox homeostasis by inhibiting the NF-ĸB and activating the Nrf2/ARE pathways. Free radical oxygen induces lipid peroxidation and conversion of AA and DHA to 4-HNE and 4-HHE, respectively [183].
Resveratrol, a stilbene formed in numerous plants in response to various stressors, produces multiple beneficial effects in vertebrates. Resveratrol was shown in particular to have therapeutic properties in cancer, neurodegeneration, and atherosclerosis. Resveratrol-induced benefits are modulated by multiple synergistic pathways that control oxidative stress, inflammation, and cell death. Despite the lack of a definitive mechanism, in vivo and in vitro studies suggest that resveratrol can induce a neuroprotective state when administered acutely or before an experimental injury to the CNS [184].
It has been verified that curcumin may prevent mitochondrial dysfunction in the brain of the senescence-accelerated mouse-prone 8 (SAMP8) strain. Thus, it can be used for nutraceutical neurodegenerative disease prevention [185].
Nutraceuticals such as alpha-lipoic acid, coenzyme Q10, nicotinamide, acetyl-l-carnitine, and polyphenols protect mitochondrial biogenesis and function and, therefore, have protective effects on cellular energy production. Dietary polyphenols/flavonoids have antioxidant and anti-inflammatory effects by decreasing the release of cytokines (IL1β, TNF-β) and inhibiting the activation of iNOS and NADH oxidase, which is released in response to glial cell activation. Flavonoids also regulate pro-inflammatory transcription factors such as NF-κB and other glial and neuronal signalling pathways that regulate stress cell ageing and immunity [186]. The structures of various nutraceuticals used in brain injury management are shown in Figure 3.
Return to play
Table 4 provides information about time management for return to play after different kinds of brain injuries.
Table 4
Information about time management for return to play after different kinds of brain injuries
| Sport | Time management for returning back | |
|---|---|---|
| Baseball | The severity of baseball- and softball-related TBIs vary considerably, from mild and returning to the field on the same day as injury, to immediate death. In a descriptive epidemiologic study examining 100 US high schools and 180 US colleges, it was found that 64.2% (1,279/1,992) of baseball players had symptoms resolved within 6 days following injury [12] Generally, when injuries were mild, players made a full recovery and symptoms resolved within one week. Moderate injuries were resolved within 7-30 days following injury. 31.7% had symptoms lasting longer than 30 days, with the exact time of symptom resolution unspecified [12] | |
| Basketball | NBA players returned to play following first-time concussion after missing 7.7 ± 8.6 days and 3.5 ± 4.1 games [21] The average games missed after a concussion from 2006 to 2010 was 1.6, significantly less than the 5.0 games missed from 2011 to 2014, following the institution of the NBA concussion protocol [24] | |
| Boxing | The whole process usually takes about 1 week, which (based on multiple studies) is the average time taken to recover from a concussion [27] | |
| Cheerleading | ||
| Cricket | ||
| Diving | Returning on the same day increases the chances of an athlete having second impact syndrome. On average, it took 23.09 days for the divers to return to practice, with a large standard deviation of 26.43 days. The average number of days before the participants returned to practice was a full week longer than the average number of days it took for the symptoms to resolve. This statistic follows the concussion management procedure used in most NCAA universities involving a seven-day, gradual, return to play protocol that begins after all symptoms have resolved [59] | |
| American football | ||
| Golf | Most patients were treated and released (93.7%) and 5.9% required hospitalisation [77] | |
| Gymnastics | Official gymnastics organisations’ websites provide no readily available data about injury rates or methods of prevention [78] Overall, injury rates were highest in freshman-eligible athletes [79] | |
| Hockey | High rates of ball-contact-related injuries resulted in time loss and medical consultations. Head injuries were frequent, however did not result in significant time loss as compared to other injuries. The use of protective gear should be recommended [87] The time from concussion to return-to-play ranged from 4 to 70 days (mean: 16.67(17.53), median: 11) in 47 Tier III Junior-A competitive ice hockey players [age 18.49(1.03)] [91] | |
| Karate | 95.2% mild: time lost lest than one week; 4.8% moderate: time lost between 1 week and 1 month; 95.1% minor: athlete able to continue competition; 4.9% time-loss: athlete forced to withdraw from competition [94] | |
| Mountain climbing | ||
| Rugby | Concussion was the most common time-loss head injury, with 1.46 per 1000 player match hours [111] The overall incidence for time-loss head injuries was 2.43 injuries per 1000 player match hours, with a higher incidence for the amateur (2.78; 95% CI: 2.37-3.20) compared with recreational (2.20; 95% CI: 1.86-2.53) (p = 0.032) playing level, but was not different from the semi-professional (2.31; 95% CI: 1.83-2.79) playing level. Concussion was the most common time-loss head injury, with 1.46 per 1000 player match hours [115] | |
| Soccer | ||
| Volleyball | The incidence of time-loss injuries during match play was 3.8/1000 player hours (95% CI: 3.0-4.5); this was greater for senior players than for junior players (relative risk: 2.04, 1.29 to 3.21) [128] | |
| Wrestling | Over one-third of patients were between 15 (17.7%; 95% CI: 15.8-19.7%) and 16 (17.0%; 95% CI: 14.9-19.1%) years of age, which comprised the peak age groups during which such head injuries were sustained [134] | |
Conclusions
Brain injuries are prevalent in sports and are difficult to manage, but athletes’ health must be the priority. Therefore, injury prevention should be essential to every physical activity because it helps to achieve athletes’ training goals and keeps them healthy and safe. Of the sports analysed, baseball, boxing, American football, ice hockey, and wrestling have particularly high incidence levels. Therefore, preventive measures in these sports should be even stricter. As for the treatment of brain injuries in sports, a comprehensive approach should be adopted. This includes using pharmacological and non-pharmacological strategies, nutraceuticals, non-invasive and invasive non-surgical interventions, and also surgical interventions, particularly in life-threatening situations.