Introduction
Falls among older adults pose a major global health concern, affecting approximately one in three individuals aged 65 and older annually. The incidence of falls rises with age, emphasising the need for preventive measures [1]. The consequences of falls include physical injuries, limitations in daily activities, loss of independence, fear of future falls, and an elevated mortality risk [2]. The ageing population and declining musculoskeletal function contribute to an increasing prevalence of fragility fractures [3]. Addressing this public health challenge requires a focus on postural stability assessment and training to enhance balance and reduce fall risks among older adults. The growing demand for effective postural stability evaluations underscores the significance of this field in modern medicine.
Postural stability, defined as the ability to control the vertical projection of the centre of gravity (coG) or the centre of pressure (coP) within a specified base of support, plays a crucial role in preventing falls [4]. Hauer et al. [5] found that a comprehensive program incorporating balance and strength training can significantly reduce fall incidence compared to a control group. Ganz et al. [6] identified pre-existing gait and balance disorders as consistent predictors of future falls, with a likelihood ratio ranging from 1.7-2.4. Screening for fall risk is complex due to multiple contributing factors, but posturographic analysis emerges as a valuable tool for identifying individuals at risk due to insufficient postural stability. Assessing balance and fall risk in older adults involves a range of methods, from simple and cost-effective assessments like the timed single-leg stance, functional reach test, sit-to-stand test, and timed up-and-go test, to more sophisticated techniques utilising specialised equipment [7, 8]. Routine assessments such as the berg balance Scale and Tinetti’s Performance-Oriented Mobility Assessment [9], along with advanced methods like dynamic posturography and motion analysis, offer comprehensive insights [10]. Dynamic posturography measures CoG’s movement through force platform measurements, while motion analysis combines motion cameras with force platform measurements for 3D motion analysis [11]. While no single approach identifies those at risk of falls, posturo-graphic analysis stands out as a promising tool for identifying individuals with insufficient postural stability.
The five times sit-to-stand test (FTSST) serves as a valuable assessment tool for gauging functional mobility in older adults by measuring their ability to repetitively stand and sit. The test relies on the individual’s balance control and lower limb muscle strength [12] and is widely used to evaluate functional mobility in older populations [13]. As identified in previous research, balance and lower limb muscle weakness are key factors contributing to falls in older adults [14]. The FTSST is cost-effective, reliable, and time-efficient in assessing sit-to-stand capacity [15]. Challenges in FTSST performance, such as decreased ability or test incompleteness, have been linked to irregularities in balance, gait patterns, and an increased risk of falls among older adults [16]. Tiwari et al. [17] found that FTSST is strongly associated with dynamic balance (r = -0.61, p < 0.001) and moderately associated with power (r = -0.52, p = 0.001). While the FTSST precisely assesses balance, it cannot quantify actual postural sway characteristics from the CoP, providing a relative measure without an absolute numerical value. Currently, no established cut-off score for CoP sway length measurements obtained through the Nintendo Wii balance board (NWBB) exists to effectively identify fall risk in healthy older adults.
The NWBB is a commercially available gaming device equipped with four weight distribution sensors to capture and analyse body movements. Functioning similarly to a force plate, the NWBB provides an immersive gaming experience where players control characters using body movements while the board measures weight distribution [18]. Force plates, the gold standard in balance measurement, are expensive and often limited to large universities, hindering their use in clinical settings. The NWBB, being a more cost-effective alternative, has the potential to screen patients and older adults for fall risk, mitigating injuries and hospitalisations. Chang et al. [18] demonstrated good reliability and validity of the NWBB in measuring centre of mass (CoM) motion, with moderate to high correlation in older adults (ICC3,j = 0.86-0.99, r = 0.58-0.86). Furthermore, Hernandez-Laredo et al. [19] highlighted that the NWBB has been designed as an affordable, IoT-enabled platform for balance assessment, offering precise CoP measurements and supporting remote monitoring and personalised interventions. Additionally, the NWBB has been utilised to assess dynamic balance during sit-to-stand movements in older adults with locomotive syndrome, underscoring the critical role of balance training in fall prevention [20]. However, its effectiveness in screening fall risk in older adults has not been explored. This study aims to establish the predictive, concurrent, and construct validity of using the NWBB to measure CoP sway length for identifying fall risk in older individuals. Specifically, the study aims to determine the optimal NWBB cut-off score for CoP sway length, explore the relationship between FTSST performance and NWBB balance, and distinguish between older individuals at risk and not at risk of falling based on Nintendo-measured postural sway.
Material and methods
Study design
Employing a cross-sectional design, sixty community-dwelling female elders from Phayao province in northern Thailand were recruited for this study. Written informed consent was obtained from all participants.
Participants
A total of 84 older adult women were engaged through targeted outreach led by community leaders and healthcare volunteers. After stringent application of inclusion/exclusion criteria, 68 participants aligned with the specified criteria, while 16 were excluded for not meeting the criteria. The excluded participants included 10 with knee osteoarthritis, 2 with rheumatoid arthritis, and 4 with a history of stroke. Consequently, from the initial pool of 68 participants, 60 older female adult participants were available for analysis, with 30 identified as fallers. Therefore, the study strategically utilised data from the remaining 30 participants, ensuring an equivalent number for the non-fallers. The flowchart reports the number of participants at each stage of the study, shown in Figure 1. The sample size determination in this study utilised G*Power software, incorpo rating mean and standard deviation values obtained from a prior investigation by Melzer et al. [21] on postural sway. A power calculation was conducted, considering a critical α-value of 0.05, with the aim of attaining a power level of 80%. The inclusion criteria encompassed individuals aged 65 and above, with a body mass index (BMI) ranging from 18.5 to 30 kg/m2, who underwent screening for demographic characteristics. Exclusion criteria were applied to participants displaying lower extremity joint inflammation or muscle pain, a diagnosis of Parkinson’s disease or stroke sequelae, reported dizziness, and uncorrectable visual or auditory deficits. Additionally, individuals with acute illness or injury, unstable heart disease, or uncontrolled hypertension were excluded from the study.
Procedures
The research involved screening eligible participants, evaluating demographic factors (age, height, weight, BMI, and leg length), vital signs, underlying conditions, and the need for a walking aid. Participants were then categorised into two groups: non-fallers and fallers, the latter consisting of those who had experienced one or more fall events in the previous six months [22]. CoP sway length variables in each direction during conditions of quiet standing were measured using the NWBB. The protocols for assessing postural sway with NWBB and conducting FTSST were as follows.
Five Times Sit-to-Stand Test (FTSST)
The study participants were directed to sit in a standard armless chair with a seat height of approximately 43 cm and instructed to cross their arms over their chests while maintaining a 100° flexion of their knee joints [23]. They were then instructed to rise from the chair with their hips and knees fully extended, rapidly return to a sitting position, and repeat this process five times. The time it took to complete five repetitions (Tsit to stand) was recorded by an assessor using a stopwatch once the participant’s back touched the chair’s backrest after the fifth repetition. The average time of three trials was noted, and a power index of the sit-to-stand test (Psit to stand) was calculated using the following equation [23]:
where 0.43 (m) represents the height of the chair, L (m) represents the participant’s leg length, which is the distance measured from the greater trochanter of the femur to the lateral malleolus, and g (9.81 m/s2) represents the acceleration due to gravity.
NWBB for assessment of postural sway during quiet standing
The NWBB is constructed from plastic composite and equipped with four load sensors located on each corner to measure vertical forces. To extract data, freely available software was utilised to interface the NWBB to a laptop via Bluetooth. A Windows laptop computer was used to stream data from the NWBB, utilising a Bluetooth protocol and customised programs. Data were sampled from the NWBB at a frequency of 30 Hz, which was selected based on the similarity to frequencies (10-50 Hz) used in previous studies [24, 25]. The signal was then low-pass filtered with a 10 Hz cut-off. The NWBB was calibrated before each trial by applying a known weight (20.4 kg) onto the board [24].
The participants completed standing trials in a randomised order across four distinct conditions to reduce bias: natural quiet standing with eyes open on a hard surface (EO/HS), natural quiet standing with eyes closed on a hard surface (EC/HS), natural quiet standing with eyes open on a soft surface (EO/SS), and natural quiet standing with eyes closed on a soft surface (EC/SS). To simulate soft surface conditions during natural quiet standing, an AIREX® balance pad (0.50 x 0.41 m; Airex AG, Inc.) was placed atop the NWBB. For the hard surface condition, participants stood directly on the NWBB without the use of a bal ance pad. Each condition was tested in two trials. During each standing trial, participants were instructed to stand in a comfortable position while maintaining eye contact on a marker placed at their preferred eye level in the eyes-open condition and before closing their eyes in the eyes-closed condition. The trials were one minute in duration. Participants were instructed to maintain a standing position with their feet aligned parallel to each other and separated by approximately 10 cm between the heels [26] while crossing their arms over the chest. The NWBB was utilised to measure the CoP sway length during quiet standing, and the recording was performed during the middle 30 seconds of the testing period. The average value of the two recordings was analysed.
Statistical analysis
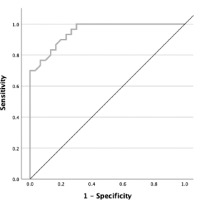
Statistical analyses were conducted using SPSS version 21 for Windows, with a significance level of p < 0.05. The Shapiro-Wilk test was employed to evaluate whether the variables followed a normal distribution. For normally distributed data, results were presented as the mean ± standard deviation (SD). The independent sample t-test was used to examine differences in characteristics, including Tsit to stand and Psit to stand, as well as CoP sway length measured by the NWBB, between older adult participants with and without fall histories. Correlations between FTSST outcomes and CoP sway length, as assessed by the NWBB, were quantified using the Pearson correlation coefficient (r). Additionally, the receiver operating characteristic (ROC) curve was used to determine the cut-off score, sensitivity, specificity, and area under the curve (AUC). The ROC curve is a statistical method used to evaluate the performance of a diagnostic test by plotting the true positive rate (sensitivity) against the false positive rate (1-specificity) at various threshold settings. Multiple cut-off scores were evaluated, each corresponding to varying levels of sensitivity and specificity. The optimal cut-off score was selected based on the highest balance between sensitivity and specificity, ensuring the best threshold for accurate outcome prediction. The AUC was also calculated to assess the model’s ability to discriminate between groups, with values closer to 1 indicating greater accuracy in distinguishing between the groups.
Results
Table 1 displays the demographic and anthropometric characteristics of the study participants. A total of sixty female older adults were enrolled, with a mean age of 71.03 ± 5.58 years. The mean weight, height, BMI, and leg length were 52.73 ± 10.20 kg, 151.97 ± 5.52 cm, 23.00 ± 3.65 kg/m2, and 83.58 ± 3.04 cm, respectively. No significant differences were observed in any of the demographic characteristics between the faller and non-faller groups (p > 0.05). The mean Tsit to stand and Psit to stand were 13.55 ± 2.00 seconds and 80.13 ± 24.38 Watts (W), respectively. The faller group exhibited significantly longer Tsit to stand and significantly lower Psit to stand compared to the non-faller group (p < 0.01), as shown in Table 1.
Table 1
Demographic characteristics and FTSST performance in older adults with and without fall histories
The length of CoP sway during quiet standing exhibited significant differences between the faller and non-faller groups in the EO/SS and EC/SS conditions in both the anteroposterior (AP) and mediolateral (ML) directions (p < 0.001). However, in the EC/HS conditions, significant differences were only observed in the AP direction (p < 0.05). The faller group exhibited a significantly greater CoP sway length compared to the non-faller group, as shown in Table 2.
Table 2
Comparison of the CoP sway during quiet standing between the faller and non-faller groups
In EC/SS and EO/SS conditions, a strong positive correlation was found between Tsit to stand and CoP sway length as measured by NWBB in both the AP (r = 0.761, p < 0.001) and ML directions (r = 0.729, p < 0.001) and in the AP direction during the EO/SS condition (r = 0.712, p < 0.001). Additionally, Tsit to stand was moderately positively correlated with CoP sway length in the EO/SS condition, ML direction (r = 0.594, p < 0.001) and in the EC/HS condition, AP direction (r = 0.468, p < 0.001), and was weakly positively correlated with CoP sway length in the EC/HS condition, ML direction (r = 0.345, p = 0.007). No significant correlations were found between Tsit to stand and CoP sway length in the EO/HS condition in either direction (p > 0.05), as shown in Figure 2.
Figure 2
Scatter plots showing the relationship between Tsit to stand and centre of pressure (CoP) sway in each condition and direction

According to the finding of the NWBB measurement of CoP sway length, the appropriate cut-off scores of AP sway in EC/SS conditions was > 3.89 cm to identify those at risk of falls with the best sensitivity (90.0%) and specificity (80.0%) with an AUC of0.949 as shown in Table 3 and Figure 3. The cut-off score of 3.89 cm was selected based on its optimal balance between sensitivity and specificity. While the 3.61 cm cut-off had the highest sensitivity (97.0%), its low specificity (70.0%) resulted in many false positives. The 3.89 cm cut-off provided a high sensitivity and specificity, making it a reliable threshold for identifying older adults at risk of falls while minimising false positives. In contrast, the 4.39 cm cut-off had higher specificity (87.0%) but lower sensitivity (80.0%), leading to missed at-risk patients (false negatives). Therefore, 3.89 cm was chosen for its balanced performance, with an AUC of 0.949, ensuring accurate identification of fall-risk individuals.
Figure 3
The receiver operating characteristic (ROC) curve of AP sway length in EC/SS measured by NWBB
Discussion
The analysis of body CoP sway reveals notable variations across both AP and ML directions. This discrepancy is particularly evident during the quiet standing test conducted on a soft surface, utilising sway length measurements obtained through the NWBB game console. The eyes closed condition, specifically during the quiet standing test on a soft surface in the AP direction, exposed a noteworthy difference of 1.65 cm between the fallers and non-fallers in our older adult groups. The variations in sway length across both AP and ML directions during the quiet standing test on a soft surface, using the NWBB game console, underscores the impact of health conditions on postural stability. The utilisation of the eyes closed condition during the quiet standing test on a soft surface adds depth to the investigation, emphasising the role of sensory input in maintaining balance [27]. The substantial difference between the two groups in the AP direction sheds light on the influence of sensory deprivation on postural control during such conditions [28]. The findings of this study unequivocally affirm the test’s remarkable capability to discern with high effectiveness between older adult individuals who face an elevated risk of falling and those who are not susceptible to such risks. This pivotal distinction underscores the test’s potential as a valuable tool in identifying and stratifying fall risk among the older adult population, offering significant implications for targeted intervention strategies and comprehensive healthcare planning tailored to individual needs. Hence, the incorporation of this test in conjunction with the NWBB demonstrates discriminative validity, establishing its capacity to effectively screen and identify older adult individuals who are at a heightened risk of falling.
CoP sway, which refers to the movement of the COP under the feet, is often analysed to assess postural control and stability in individuals, particularly in the context of fall risk among older adults [29, 30]. The differences in CoP sway between fall-risk and non-fall-risk older adults in both the AP and ML directions can be attributed to various factors related to age-related changes, sensorimotor functions, and musculoskeletal conditions [31, 32]. Fall-risk older adults often experience muscle weakness and imbalances, especially in the lower extremities. These factors can lead to difficulties in maintaining an upright posture and contribute to increased CoP sway in both AP and ML directions [33]. Ageing significantly impacts the nervous system, particularly in terms of nerve conduction velocity (NCV) and sensory input processing [34, 35], including vision, proprioception, and vestibular function. Impaired sensory input can disrupt the ability to perceive and respond to changes in body position, leading to increased coP sway as individuals struggle to maintain stability [28, 36]. Ageing is associated with joint stiffness and reduced flexibility. Limited range of motion in joints can impact the ability to make subtle adjustments to maintain balance, resulting in greater coP sway [37]. cognitive functions, such as attention, executive function, and information processing, play a crucial role in postural control. cognitive decline, which is common in older adults, can affect the ability to coordinate movements and respond to environmental cues, contributing to increased coP sway [38]. individuals at higher risk of falling may develop a fear of falling, leading to cautious and stiff movements. This fear and altered movement patterns can increase coP sway as they may overcompensate for perceived instability [39]. it is important to note that these factors are interconnected, and a comprehensive assessment is often needed to address the multifaceted nature of fall risk in older adults.
This demonstrates discriminative validity in assessing fall risk. Research has shown its ability to distinguish between older adult individuals who have experienced falls and those who have not based on coP data [40]. Additionally, studies have validated the Wii balance board’s effectiveness in assessing static balance and detecting the impact of dual-task activities on balance in healthy participants [41]. The concurrent and discriminant validity has been confirmed through Wii Fit assessments, indicating its reliability in evaluating balance activities [42]. Overall, the Wii Balance Board is a promising tool for fall risk assessment, especially in post-stroke patients [43]. in the present investigation, a noteworthy disparity in coP outcomes emerged between cohorts of older adults categorised as either at risk of falling or not. These findings underscore the robust discriminative validity of the coP sway test conducted with the NWBB, aligning consistently with outcomes observed in prior research.
The investigation additionally revealed that coP sway, particularly in the eyes-closed condition and on soft surfaces during the quiet standing balance test, demonstrated a significant and strong positive correlation with the FTSST (r = 0.729 to 0.761). FTSST is a widely employed measure for assessing balance proficiency in older adults. The study indicates that the coP sway test utilising the NWBB not only exhibits robust concurrent validity, positioning it as a viable alternative to the FTSST, but offers the distinct advantage of quantifying true balance values numerically. It is noteworthy; however, that this test does not serve as a functional assessment. The literature consistently supports the concurrent validity of the NWBB in assessing the coP in older adults. Multiple studies conclude that the NWBB is a valid tool for evaluating standing balance. Its portability, widespread availability, and cost-effectiveness make it a practical choice for assessing coP in older adults [44, 45]. Furthermore, a systematic review reinforces the reliability and concurrent validity of the NWBB for static standing balance assessment [46]. Overall, the evidence suggests that the NWBB can be considered a reliable and valid instrument for evaluating standing balance and sensory integration in highly functional older adults. This study uniquely focuses on concurrent validity, deviating from prior research. The investigation extends its exploration to determine an optimal cut-off score for distinguishing older adult individuals prone to falling from those not at risk. Notably, utilising the NWBB during a quiet standing balance test, with Ec/SS and assessing the AP sway variable, emerges as the most effective approach. A pivotal finding reveals that an AP sway exceeding 3.89 cm during the test indicates a 90.0% likelihood of falling for older adult individuals. This high sensitivity implies the test’s capability to detect seventy-three out of one hundred older adults at risk of falling. Additionally, the test demonstrates a specificity value of 80.0%, enabling the identification of around fifty-seven older adults from one hundred older adults not at risk of falling. This level of accuracy deems the test suitable for effectively screening the risk of falling among older adult community members.
Nevertheless, this study presents certain limitations that warrant acknowledgement. The investigation predominantly concentrates on the AP and ML dimensions in coP sway, placing a distinct emphasis on soft surface conditions. Notwithstanding, the exploration of other potentially influential variables, such as psychological factors or specific health conditions, remains relatively cursory. This restricted focus has the potential to curtail the comprehensive understanding of fall risk determinants among older adults. Furthermore, this study is limited by its focus on a specific demographic, as all participants were older adult females. This was due to the higher prevalence of falls among older women, which may limit the generalisability of the findings. Additionally, the homogeneity in terms of age, health status, and cultural background further narrows the applicability of the results. Future research should include male participants and more diverse populations to explore potential gender-related differences and enhance the broader relevance of the findings.
Conclusions
This research, utilising the NWBB, highlights significant variations in coP sway during the quiet standing test on a soft surface. The study emphasises the impact of older adult health conditions on postural stability. The coP sway test effectively discerns older individuals at risk of falling, showcasing its potential for targeted fall risk identification. This study provides valuable insights into fall risk assessment, emphasising the effectiveness of the NWBB. It serves as a practical tool for identifying older adult individuals at risk of falling, offering implications for tailored healthcare planning.



