Introduction
Humeral fractures account for 7.4% of all fractures in adults, with shaft fractures being the second most common in this population behind proximal humeral fractures, which represent 5.7% of all humeral fractures [1-3]. The most common mechanisms for shaft fractures are falls, especially in women aged over 50, and automobile accidents, which predominantly affect young males aged 20 to 30 [3, 4].
Two treatment approaches are used for humeral shaft fractures, including non-invasive conservative immobilisation and open reduction internal fixation [5-7]. Regardless of the treatment used, recovery of phys - ical function in the postoperative period depends entirely on physical therapy intervention. Indeed, the longer the delay in receiving physical therapy, the slower the re covery of a patient’s functional performance in their daily activities [8].
Physical therapy helps improve the range of motion (ROM), functional capacity, and muscle strength, as well as helping to control pain [9-11]. The benefits of this intervention are related to preventing and treating complications from the immobilisation period since it is associated with the development of kinesiophobia, joint stiffness, fibrosis of structures adjacent to the injury, changes in electrical muscle stimulation, and muscle atrophy, characterised by reduced strength and muscle cross-sectional area [12, 13].
Land-based exercises are usually the first option for postoperative treatment of upper limb fractures. However, aquatic physical therapy or aquatic exercise (AE) is already considered an effective post-surgical treatment option for other dysfunctions, such as ante- rior cruciate ligament reconstruction, post-cancer mastectomy, and lumbar spine surgeries [14-16]. Therefore, AE may be a beneficial initial intervention for individuals with upper limb fractures, as it has been shown to be an effective and safe treatment modality after orthopaedic surgeries. AE offers greater comfort for exercising during the initial post-surgery phase and does not increase the risk of adverse events related to the surgical wound. Furthermore, it does not differ from land-based therapy in the immediate postoperative period in terms of pain, oedema, and ROM [17].
However, the literature on the effects of AE in the postoperative treatment of fractures and upper limb surgeries in general is scarce. Therefore, to explore this issue and analyse/validate the results of AE in individuals affected by this condition, robust analytical approaches are needed to evaluate clinical results over time. Simulation Modeling Analysis (SMA) is a promising tool in this context. Using the bootstrap method, which involves random resampling of the original dataset, allows for more reliable and robust estimates. As a result, SMA typically provides more accurate outcomes than other inference methods and enables analysis even in studies with small sample sizes, as seen in previous case reports [18, 19]. Therefore, the current case report aimed to simulate the results ofphysical function through SMA and analyse possible changes in the minimal clinically important difference (MCID) in an individual with a humeral shaft fracture after undergoing AE alongside some land-based exercises.
Material and methods
Subject characteristics
A 46-year-old male patient with a body mass index of 26.42 kg/m2 was referred for evaluation at the Laboratory of Biomechanics and Clinical Epidemiology at the University Hospital/UEL in the immediate postoperative period after fixation of a greater tuberosity fracture and diaphysis of the humerus in his left limb (non-dominant). During the waiting period before the surgery (six days), the individual had an improvised splint made by the paramedics. As this fixation was inappropriate, the patient developed pressure ulcers of the medial epicondyle and costal margin regions, both on the left side. The patient underwent open reduction internal fixation with intramedullary nail fixation six days after the fracture.
One day after the surgical procedure, the patient was discharged from the hospital and started wearing a sling for immobilisation, which was maintained for six weeks post-surgery because they reported pain and fear when attempting to move the left upper limb. The fact that the affected limb was not the dominant side contributed to the longer immobilisation time. After this six-week period, the patient had a follow-up appointment with the doctor who performed the surgical procedure and was cleared and referred to begin the treatment.
The initial contact with the patient occurred in the immediate postoperative period. After receiving the necessary information and signing the informed consent form (#171138413.1.0000.5231), approved by the Institutional Review Board (UEL), the participant responded to five Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) pre-intervention questionnaires. Following these procedures, the patient was assessed and treated with AE (n = 15) and land-based exercises (n = 5).
Initial examination/clinical measures
The patient was assessed through an anamnesis (personal data, injury history, and main complaint) and underwent inspection, palpation, and bilateral perimetry of the upper limbs and shoulder girdle to obtain parameters for comparison. The pre-intervention assessment was conducted six weeks postoperatively, and the reassessment was carried out 10 weeks after the surgery.
Physical function
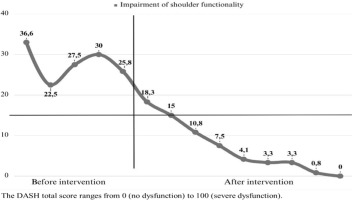
The outcome of functional capacity was assessed using the DASH questionnaire, which has well-established validity in the Portuguese language and reproducibility in the literature [20]. DASH consists of 30 self-reported items for measuring physical incapacity and symptoms of upper limb dysfunction. The DASH score ranges from 0 to 100, with 0 indicating the lowest degree of disability and 100 indicating the highest, and is calculated using established formulas [20]. In addition, the MCID was assessed, which is defined as the smallest difference in the score that patients perceive as beneficial, capable of detecting small but significant changes in health status over time [21, 22]. The expected MCID reported in the literature for the DASH questionnaire ranges from 8.1 to 13 points [23].
Muscle performance - dynamometry
Muscle strength was measured using the MicroFet 2 HHD portable dynamometer (Hoggan Health Industries, UT, UsA) by performing the maximum voluntary isometric contraction, and the values were presented in kilograms-force (kgf). Three consecutive tests were carried out for each muscle, with a 60-second interval between them. The highest result was considered as a reference for data analysis. For each strength test, the participant was instructed to exert maximum effort against the resistance applied by the evaluator for five seconds [24]. Instead of the evaluator applying force with the “breaking” technique or overcoming the participant’s resistance, as is common in manual strength tests, the participant exerted force against the dynamometer, which is considered a more reliable technique [25, 26].
The participant was instructed on each movement and performed three submaximal efforts with a 60-second rest interval for each tested muscle group, which familiarised them before tests were carried out [27]. The muscle groups tested bilaterally included shoulder abductors, flexors, extensors, external and internal rotators, and elbow flexors and extensors.
Range of motion
ROM was measured using a manual goniometer and carried out by the same independent evaluator. The analysed movements included shoulder flexion, extension, internal rotation, external rotation, abduction, and adduction, as well as elbow flexion and extension. The assessment helps determine the presence or absence of dysfunctions, quantifies limitations of joint angles, and makes it possible to compare the initial assessment with future reassessments. The evaluator used predetermined anatomical points as references, and the participant was instructed to wear clothing that allowed easy access to the anatomical structures being analysed. Before beginning the assessment, the procedure was clearly explained with the execution of the passive movements, and ROM was performed through the execution of the active movements [28]. The patient was positioned to avoid any form of compensation, and the evaluation was carried out bilaterally to enable comparisons.
Intervention
The treatment lasted 11 weeks, consisting of 15 AE sessions and five land-based sessions performed at the beginning of treatment (two initial weeks), totalling 20 sessions. The AE sessions were conducted in an Aquatic Physical Therapy Center “Prof. Paulo A. Seibert” HU/UEL. The pool used for these sessions was indoor and heated, with an average temperature of 32.5°C, dimensions of 15 x 13 x 1.30 m, and a water depth of 1.20 m.
The sessions were divided into three parts, including warm-up, mobilisation, and resistance exercises. The procedures performed in each session are described in Tables 1 and 2.
Table 1
A description of the aquatic exercise intervention
Table 2
A description of the land-based exercise intervention
Simulation modeling analysis
The data from the DAsH questionnaires were analysed with sMA, which uses the resampling method to calculate a randomly generated sample of 5000 cases from the initial sample. Through the bootstrapping method, sMA examines short, autocorrelated data, and generates simulated data sets that replicate the original series’ autocorrelation and size (DAsH scores in this study) and applies Crosbie’s small sample bias correction [29].
A correlation coefficient was computed against the intervention phase vector for each simulated autocor- related series. Any coefficient surpassing the correlation of the original data with the phase vector was marked and counted. In this way, sMA answers the question, what is the probability that a random data series, matching the length and autocorrelation of the original series, will exhibit as strong a correlation with the phase vector as the original? [19].
The sMA method controls Type I errors and reliably detects small effect sizes, achieving a power of 0.80 with at least five data points per phase for a five standard deviations effect [30]. sAM is ideal for time-series studies, in which, as in the case of the current study, physical function on one day partially influences the subsequent days, making data points interdependent [19].
The analysis is dependent on a lag, dividing the series into pre and during-intervention phases. The preintervention phase included the five questionnaire responses (48 h apart), while the intervention phase covers one questionnaire response per week. Autocorrelation between the two periods was assessed to measure its similarity.
The Pearson correlation coefficient (r) explored the relationship between physical function and intervention duration. If p < 0.05, the function can be predicted by intervention weeks. The slope, which represents the average predicted change in y per unit increase in x, was analysed to determine the curve inclination and physical function improvement in each week of treatment.
Results
Physical function was assessed using the DAsH questionnaire, and the results revealed a reduction between pre-intervention and post-intervention values (18.3% and 0% impairment, respectively) (Figure 2). Furthermore, when analysing the correlations between the randomly generated variables in the time series program, a correlation was observed between the physical function values (autocorrelation coefficient = -0.78, r = -0.87, and p = 0.010) and the slope representing the curve inclination was = -2.25 points (p = 0.008). The upper limb circumference is presented in the table 3. ROM improved in all shoulder movements, including flexion (initial: 52°; final: 140°), extension (initial: 30°; final: 45°), abduction (initial: 58°; final: 110°), internal rotation (initial: 64°; final: 90°), and external rotation (initial: 0°; final: 32°). Additionally, elbow ROM increased by 25%, from 112° to 140° (Table 4). shoulder flexor muscle strength increased from 3.9 kgf in the initial assessment to 11.7 kgf in the final assessment. Likewise, the elbow flexors showed a significant increase in strength, from 18.8 kgf to 30.2 kgf (Table 5).
Table 3
Upper limb circumference in centimetres (cm)
| Involved (left arm) | Uninvolved (right rm) | |||
|---|---|---|---|---|
| 10 cm below | 20 cm below | 10 cm below | 20 cm below | |
| First assessment | 28.5 | 31.7 | 28.6 | 33.2 |
| Revaluation | 34.0 | 29.5 | 34.0 | 29.5 |
| Final assessment | 34.2 | 28.6 | 35.8 | 29.5 |
Table 4
Shoulder range of motion (°)
Discussion
This study assessed physical function, ROM, and muscle strength in an individual with a humeral shaft fracture after undergoing 15 sessions of AE and five land-based sessions. Physical function values were assessed using the DAsH questionnaire, with positive results, and the MCID was reached, where 75 % of the variation in the DAsH values was accounted for by the number of weeks of treatment (p = 0.008). A slope of -2.25 was found, meaning that for every one- unit increment in the DASH questionnaire, the predicted value of the dependent variable (# of weeks of treatment) was anticipated to decrease by 2.25 points.
AE is described in the literature as an effective modality in the post-surgical treatment of various conditions, such as anterior cruciate ligament reconstruction, post-cancer mastectomy, and lumbar spine surgeries [14-16]. The benefits of AE during the postoperative period may be associated with the various physiological changes induced by the aquatic environment on the human body, resulting from fluid mechanics. The effects of temperature and hydrostatic pressure favour oedema reduction by increasing venous return and lymphatic drainage [31]. In addition, immersion in heated water can reduce postoperative pain, and performing exercises in the water provides greater comfort for patients during the initial post-surgery treatment phase [17, 32]. Thus, using AE during the postoperative period of upper limb fractures may be a viable option for these patients.
Humeral shaft fractures are associated with changes in shoulder and elbow ROM [33]. Possible consequences of surgical correction of the fracture with a humeral intramedullary nail are shoulder stiffness, subacromial impingement, and postoperative pain [34, 35]. Such changes occur due to rotator cuff tendinopathy resulting from the surgical procedure [34, 36], which was evident in the current study. The patient did not have an intra-articular fracture, though the adjacent joints were compromised, which was apparent from the values for shoulder and elbow ROM in the initial assessment (Table 4).
Physical therapy can contribute to the treatment of such complications, as some studies suggest that exercises, mobilisation, and manual therapies can be beneficial and effective treatments for rotator cuff tendinopa- thies and subacromial impingement, particularly through improving physical function and pain [37-41]. Moreover, AE has been shown to be an equivalent intervention to land-based therapy in terms of ROM, function, and pain during the postoperative period of rotator cuff injury treatment [42].
These assertions corroborate the findings of the present study since the functional values quantified by DASH showed an 18.3 % improvement (Figure 2), and the questionnaire score reached zero, indicating full functional recovery. These results exceeded the expected MCID values described in the literature for the DASH questionnaire, which range from 8.1 to 13 points for humeral fractures [23]. Furthermore, when analysing randomly generated variables with time series analysis, an autocorrelation of -0.78 was reached, indicating a strong similarity between the patterns observed before and after the start of treatment. In other words, the physical function values after the start of treatment were influenced by the pre-intervention values, generating persistent results that did not change drastically between the two time periods. Thus, physical function in a given week depends, to a large extent, on the gains achieved in the previous days/weeks. As such, if a patient consistently improves their physical function by one point per week, this autocorrelation pattern may indicate that the treatment is working as expected.
When observing the average scores between the two phases, the patient presented an average of 28.5 points (SD = 4.76) in the pre-intervention period. Functional impairment is expected immediately after surgery, mainly due to the use of a sling, immobility, and the absence of an intervention. However, after the beginning of the intervention, the average score decreased to 7.03 points (SD = 6.05). This decrease in the mean is desired and shows a good patient response to treatment, with a considerable decrease in the questionnaire values compared to the pre-intervention phase.
The prediction of physical function through the number of weeks of AE was achieved, with an r = -0.87 (p = 0.01), indicating a negative correlation since the questionnaire score decreased over time. In other words, the physical function and number of weeks of treatment variables presented a shared variance of 75%. The slope value was -2.25 per week and statistically significant (p = 0.008). Based on this finding, it was possible to calculate the number of points the patient would reduce in the questionnaire each week of treatment using the formula y = a + b-x, where y is the dependent variable (physical function), x is the independent variable (weeks of treatment), a is the intercept (the mean value of response y when x is equal to zero), and b is the slope of the curve.
The combination of AE (n = 15) and land-based therapy (n = 5) was a viable treatment for the rotator cuff after surgical repair, resulting in faster restoration of shoulder flexion ROM and improved passive ROM in other movements of this joint. Additionally, it achieved values similar to conventional treatment for shoulder function [43], which may contribute to the treatment of the aforementioned post-surgical alterations.
Likewise, after the intervention described in this case report, the results demonstrated improved ROM for all shoulder and elbow movements analysed (Table 4). There were improvements in flexion, extension, abduction, internal rotation, external rotation, and elbow ROM. These results suggest that combining therapeutic modalities in the postoperative treatment of humeral fractures can be an effective alternative for reducing motion limitations.
Open and closed kinetic chain exercises and ROM exercises have been shown to be effective in reducing pain and improving the physical function of individuals with rotator cuff tendinopathy and impingement syndrome [44]. Thus, the aquatic environment facilitates the execution of these and other activities. Vertical exercises performed in shallow water are generally related to a closed kinetic chain exercise approach, although the opposing resistance of buoyancy reduces the load on the joints. In contrast, horizontal exercises performed at the water surface and exercises in floatation or with resistors (such as hand paddles) resemble an open kinetic chain system [31].
However, land-based exercises may be more advantageous for gaining muscle strength. This conclusion is generally based on the fact that when a body is submerged, the buoyancy caused by the volume of displaced liquid opposes the force of gravity, making the load appear lighter [45, 46]. In addition, eccentric contraction may be less effective in water, as the force produced by the muscle depends on the velocity at which its fibres are stretched. As stretching velocity increases, muscle force also may increase [47, 48].
Despite these issues, the results demonstrate an increase in strength in the shoulder flexor muscles (3.9 kgf to 11.7 kgf) and elbow flexors (18.8 kgf to 30.2 kgf), as described in Table 5. These findings may be explained by the fact that muscle tissue responds to the demands imposed on it [49-51]. Even if the surgical procedure to correct a fracture is performed as quickly as possible, the patient’s affected limb remains immobilised for a minimum of five weeks [8]. During this period, disuse or decreased overload can lead to loss of muscle mass, and negative alterations in neuromuscular junctions can be observed as early as three to 10 days after the decrease in loads placed on the muscle [52, 53].
Therefore, exercises performed in water promote muscle contractions that can stimulate the activation of neuromuscular junctions and reduce disuse-related alterations while imposing a greater load on the tissues than that received during immobility but smaller than that of land-based exercises. Thus, AE can be used as an initial muscle-strengthening approach for the upper limbs. Indeed, research supports the use of carefully structured AE, with adequate control and progression of intensity and overload, to gain muscle endurance in other conditions affecting the lower limbs [54-57]. The improvement found in muscle strength was also confirmed by the circumference values, which showed an increase in both upper limbs in the proximal region of the arm after the intervention (Table 3), revealing a possible gain in the bilateral tropism of the shoulder muscles.
Despite the positive results, this study had some limitations, including variations in the number of weekly appointments caused by the daily routines of the therapist and the patient. Another limitation was the lack of assessment of muscle strength in elbow extension and other shoulder movements (external and internal rotation, extension, adduction, and abduction) in the initial assessment.
Conclusions
The results demonstrate that it is possible to predict physical function through time series analysis, with a high correlation and a slope of -2.25 each week, following combined AE and land-based exercises performed in the postoperative treatment of a humeral shaft fracture. Furthermore, a score of zero on the DASH questionnaire satisfied the MCID and indicated full physical function recovery. In addition, there was a significant improvement in muscle strength and shoulder and elbow ROM.